Oncologist: Anlotinib(安罗替尼)联合S-1三线或后线治疗晚期NSCLC患者的疗效和安全性:II期临床研究
2021-11-29 yd2015 MedSci原创
研究表明,anlotinib(安罗替尼)与S-1联合用于IV期NSCLC的三线或后期治疗,显示了良好的抗肿瘤活性和可控制的毒性。
Anlotinib(安罗替尼)是一种口服多靶点酪氨酸激酶(TK)受体抑制剂。III期临床研究ALTER-0303表明,相对于安慰剂,anlotinib(安罗替尼)在三线治疗晚期NSCLC的ORR和DCR均有显著提高(ORR 9.18% vs. 0.7%, p < .0001; DCR 80.95% vs. 37.06%,p < .0001)。同时显著改善患者预后(PFS 5.37 vs. 1.40个月, p < .0001; OS 9.63 vs. 6.30 个月,p < .0001)。基于该研究成果,anlotinib(安罗替尼)在中国被批准用于三线晚期NSCLC。但是我们也知道,anlotinib单药治疗的ORR只有9.18%,中位OS只延长3个月。因此,来自绵阳中心医院和川北医学院附属医院的团队开展了一项II期临床研究,评估anlotinib(安罗替尼)联合S-1三线或后线治疗晚期NSCLC患者的疗效和安全性。相关结果发表在Oncologist杂志上。
该研究是II期,单臂、前瞻性临床研究(Number: ChiCTR1900020948)。选取了四川省绵阳市中心医院经细胞学或组织学证实的IV期NSCLC患者。纳入标准如下:(a) 18岁-75岁;(b)病理诊断为IV期非小细胞肺癌;(c)ECOG评分0-2分;(d)对EGFR/ALK突变患者进行至少一种化疗和TKI治疗后疾病进展,以及对驱动突变阴性的患者进行至少两种化疗后疾病进展;(e)根据RECIST 1.1标准有可测量的病变;(f)预期生存时间>12周;(g)主要器官功能正常。
给药方案:安罗替尼 12mg/次/天,服用2周,休息1周,21天为一周期,直至疾病进展或死亡;S-1 70 mg/m 2,一天两次,服用2周,休息1周,21天为一周期,最多6周期。
主要研究终点为ORR,次要研究终点为DCR、无进展生存期(PFS)、总生存期(OS)和安全性。
研究纳入29例患者,其中男性24例,女性5例。中位年龄为58岁。既往全身治疗线数中位数为2 (2–5)。ECOG 0分有10例患者,1分有9例,2分有10例。腺癌有22例,鳞癌5例,腺鳞癌2例。
研究达到了主要研究终点,29例患者的ORR为30%,其中无患者达到CR,11 (37.90%)例患者PR,7 (24.05%)例患者SD,而7 (24.05%)例患者PD。DCR为62.1%。排除4例(13.8%)因不良反应而未进行基线后评估的患者,25例至少进行过一次基线后评估的患者的ORR为44%,DCR为72%。
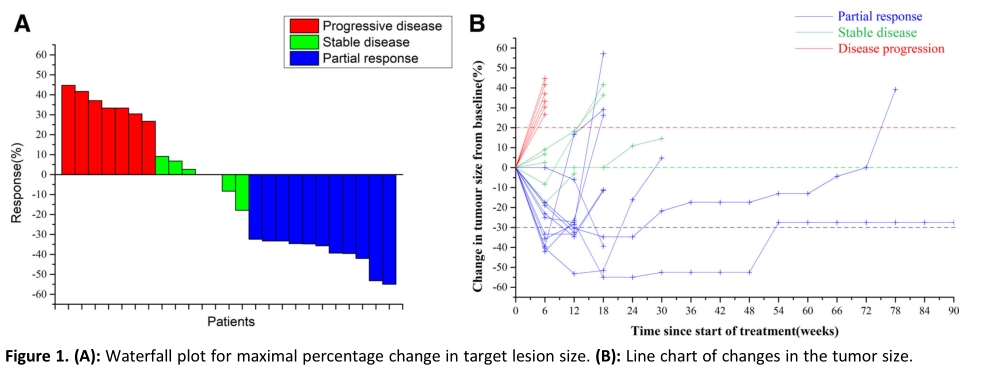
疗效评估
中位无进展生存期(PFS)为5.8个月,中位总生存期(OS)为16.7个月。
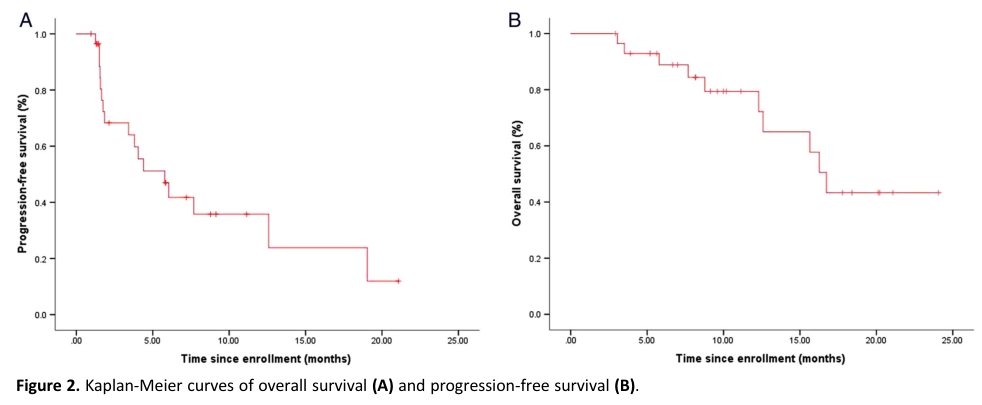
PFS和OS
最常见的3级不良事件(AEs)为胃肠道(3例[10.3%])、疲劳(2例[6.9%])和高血压(2例[6.9%])。大多数AEs是可逆的。此外,没有4级治疗相关AE或死亡记录。毒副作用可控,联合治疗未明显增加不良反应。
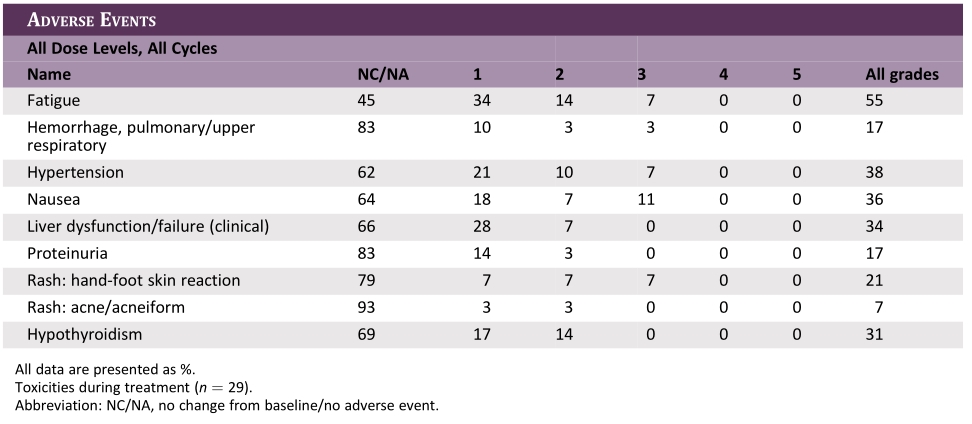
AEs
综上,研究表明,anlotinib(安罗替尼)与S-1联合用于IV期NSCLC的三线或后期治疗,显示了良好的抗肿瘤活性和可控制的毒性。
原始出处:
Xiang M, Yang X, Ren S, Du H, Geng L, Yuan L, Wen Y, Lin B, Li J, Zhang Y, Feng G, Du X. Anlotinib Combined with S-1 in Third- or Later-Line Stage IV Non-Small Cell Lung Cancer Treatment: A Phase II Clinical Trial. Oncologist. 2021 Aug 22. doi: 10.1002/onco.13950. Epub ahead of print. PMID: 34423518.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#I期临床#
57
#疗效和安全性#
45
#II期临床研究#
50
#SCLC患者#
60
#Oncol#
42
学习了
57
#NSCLC患者#
40
#晚期NSCLC#
50
#GIST#
35
#S-1#
59