PLoS ONE:质子泵抑制剂或增普通人群心肌梗死风险
2015-06-12 大鹏 译 医学论坛网
斯坦福大学研究团队近期刊登于《公共科学图书馆期刊》(Plos One)的试验结果显示,质子泵抑制剂(PPI)对血管功能有负面影响,并由此导致一般人群的心肌梗死风险升高。 虽然此研究并不是一项随机对照试验,但研究者入组了足够大的样本量保证了数据可靠性。通过药物安全数据库,研究者调取了来自290万例个体的1600万分临床档案,并将相关数据整理入组研究。
斯坦福大学研究团队近期刊登于《公共科学图书馆期刊》(Plos One)的试验结果显示,质子泵抑制剂(PPI)对血管功能有负面影响,并由此导致一般人群的心肌梗死风险升高。
虽然此研究并不是一项随机对照试验,但研究者入组了足够大的样本量保证了数据可靠性。通过药物安全数据库,研究者调取了来自290万例个体的1600万分临床档案,并将相关数据整理入组研究。同时研究者采用了称为“新型统计途径”的数据挖掘法完成了试验。
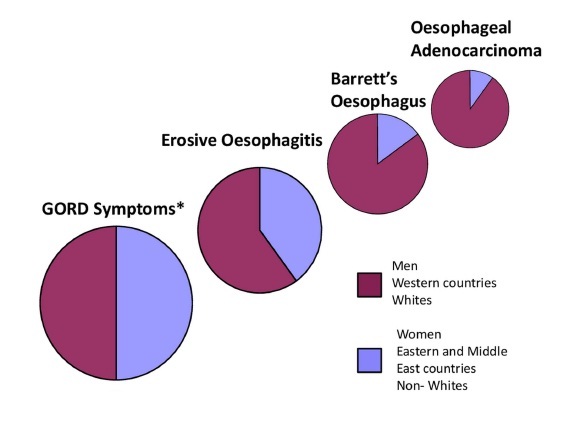
根据统计结果,研究者指出服用PPI的胃食管反流患者心肌梗死风险将升高16%,同时其心血管死亡风险升高一倍。对于“PPI可能仅是身体虚弱群体的一个侧面反映”这种假说,但研究者表示可能性不大,因为研究同时显示H2受体阻滞剂与心肌梗死风险无相关性。
机制与意义
该研究将PPI的升高心梗风险作用从冠心病患者群体扩展到了一般人群,这足以引起临床医生的重视。在机制方面,研究者认为“PPI很可能通过新机制导致心肌梗死风险升高,这种机制不是直接促进血小板聚集,而相关研究显示的PPI抑制二甲精氨酸酶作用或可解释这种现象,即使是在未应用氯吡格雷的个体中也是如此。”二甲精氨酸酶是维持心血管健康所必需的一种酶,介导非对称性二甲基精氨酸代谢,后者是一氧化氮合成酶的内源性竞争型抑制物。这就意味着PPI或调控体内一氧化氮合成,影响心肌梗死风险。
但该研究还不足以撼动PPI临床常用药物的地位,其研究结果更多的是提示临床医生注意评估患者服用该药物的风险收益比,加快PPI药物安全性试验进程。
原始出处:
Lara C. Pullen, PhD.Chronic Use of Proton Pump Inhibitors Increases Heart Risk.MedScape, June 10, 2015.
Nigam H. Shah, Paea LePendu, Anna Bauer-Mehren et al.Proton Pump Inhibitor Usage and the Risk of Myocardial Infarction in the General Population.PLoS One, June 10, 2015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Plos one#
27
#抑制剂#
27
#质子泵#
31
挺好
110
看看
91
期待着
118
新的文章
52
好的思想
109
#普通人群#
32
谢谢作者
68