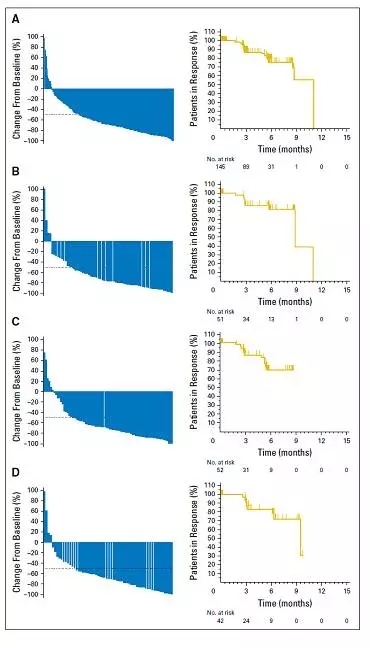
Blood : pembrolizumab治疗B细胞淋巴瘤的安全性和耐受性
2017-07-24 Yara MedSci原创
使用pembrolizumab阻断PD-1对rrPMBCL具有可控的安全性和理想的抗肿瘤活性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#细胞淋巴瘤#
24
#mAb#
0
#Pembro#
34
#PE#
26
#Pembrolizumab#
36
#B细胞#
29
#耐受性#
20