JAHA:左心室舒张功能正常的患者肺动脉高压与全身动脉高血压相关
2021-12-08 MedSci原创 MedSci原创
无论左心疾病状态如何,肺动脉高压都与全身性动脉高血压相关。这种关联在女性中更为明显。
肺动脉高压和全身动脉高压之间的关联被认为是通过高血压左心疾病介导的。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究的目的是调查肺动脉高压是否与左心室舒张功能正常的患者全身动脉高血压相关。
研究人员连续招募了2007年至2019年间进行超声心动图检查的患者。患有已知的与肺动脉高压相关的疾病状态的患者,包括舒张功能障碍,被排除在该研究的分析之外。研究人员从超声心动图检查报告中提取所有患者估计的右心室收缩压。肺动脉高压被定义为估计的右心室收缩压40mmHg以上。研究人员采用多变量Logistic回归模型进行了分析。
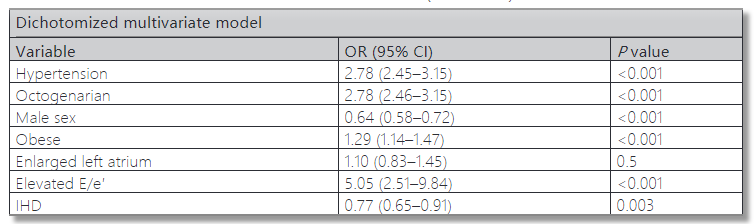
最终的研究人群包含25916名中位年龄为59(四分位距为44-69)岁的患者,其中12501名(48%)患者为男性,13265名(51%)患者伴有全身性动脉高血压。与血压正常的患者相比,高血压患者发生肺动脉高压的可能性高出3.2倍(95%CI为2.91-3.53;P<0.001)。对已知的与肺动脉高压相关的临床和超声心动图参数进行调整的多变量模型表明,高血压患者患肺动脉高压的可能性几乎是其3倍(95%CI为2.45-3.15;P<0.001)。这种关联在多个亚组中显著,但在女性中比男性更为显著(比值比为3.1 vs. 2.4;交互作用P<0.001)。
由此可见,无论左心疾病状态如何,肺动脉高压都与全身性动脉高血压相关。这种关联在女性中更为明显。
原始出处:
Edward Itelman,et al.Pulmonary Hypertension Is Associated With Systemic Arterial Hypertension Among Patients With Normal Left Ventricular Diastolic Function.JAHA.2021.https://www.ahajournals.org/doi/10.1161/JAHA.121.023603
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#舒张功能#
53
#动脉高压#
31
#AHA#
33
#左心室#
43
学习
57
哦了volleyball?V5咯哈8起Kodak。
61