ASC:太震惊了!伤口敷料能变色检测感染!
2015-11-16 chenshuo译 MedSci原创
烧伤患者除了存在明显的痛苦之外,开放性的伤口极其容易导致感染从而危及患者的生命。同时,重大的热损伤还可以诱导免疫抑制状态,进一步增加患者感染的机会。
目前,创面烧伤在国际上仍然是最常见的疾病之一。
烧伤患者除了存在明显的痛苦之外,开放性的伤口极其容易导致感染从而危及患者的生命。同时,重大的热损伤还可以诱导免疫抑制状态,进一步增加患者感染的机会。
据不完全统计,众多的烧伤患者死亡原因多是由于治疗后期得了败血症,再加上轻微的感染即可延长住院时间,增加了患者的住院费用。
现今,对于烧伤的患者是否发生了细菌感染,依当今的医疗水平,仍然难以轻易地做出诊断。一般需要大约48小时才能对烧伤患者发生感染做出明确的诊断。
为了能提早发现烧伤患者的感染情况,Amber Young博士参与了相关的临床试验。
最近,巴斯大学的研究人员与布莱顿大学的烧伤研究中心研究人员已经开发出了一种新技术解决了这个历史性的难题。
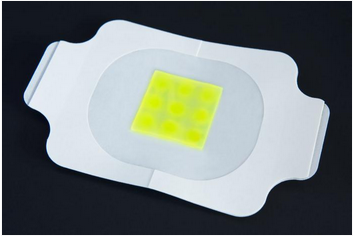
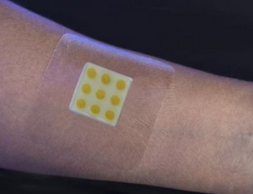
该团队开发出一种原型敷料,用于覆盖伤口表面皮肤,当伤口发生感染时,该敷料的颜色即会发生改变。未受感染的区域上的伤口敷料会显示一个离散的圆形图样。
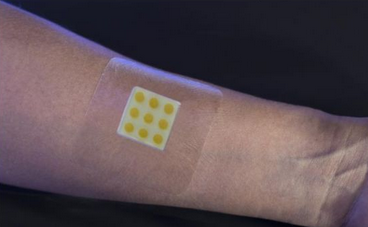
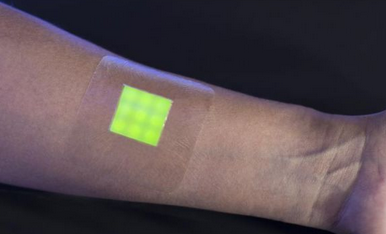
该项研究的负责人Toby Jenkins博士说, “我们的医用敷料的作用机制是---由致病细菌分泌的毒素引发伤口内的纳米胶囊释放出荧光染料。而正常的菌群则没有收到任何的影响。
而研究团队开发出的这种敷料能够检测出这些生物膜上的致病细菌。同时,敷料能特异性地识别大肠杆菌、铜绿假单胞菌、金黄色葡萄球菌和肠球菌。因此,该敷料不仅能识别出创面伤口发生了感染,还能识别出感染的个别细菌种类。
目前,该伤口敷料还处于开发的早期阶段,但很快将会被用到临床上的实际患者进行测试。
Color changing Band-Aid gives early warning of infection MNT 15 Nov 2015
N.T.Thet,D.R.Alves,et al,Prototype development of the intelligent hydrogel wound dressing and its efficacy in the detection of mode,ACS Applied Materials and Interfaces .2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












文章真好,喜欢阅读
84
继续学习
80
继续关注
92
继续学习
97
继续关注
78
#敷料#
44
#ASC#
35
楼主给力
95