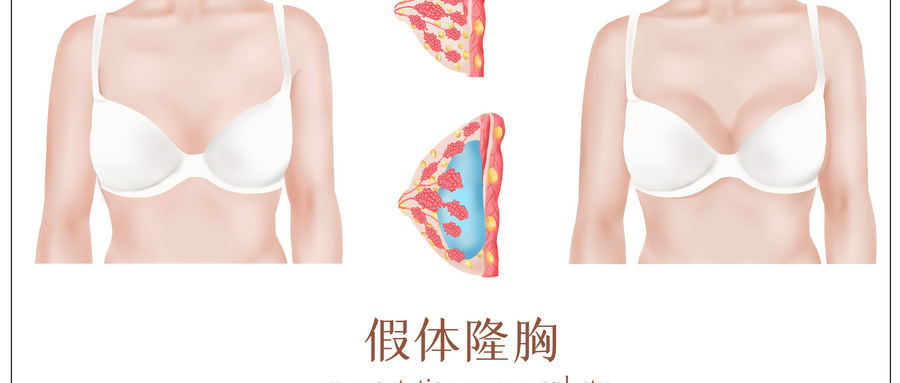
Aesthetic Plast Surg :隆胸患者植入物相关感染的治疗方案选择
2021-10-10 医路坦克 MedSci原创
隆胸手术是最常见的美容整形手术,发生率从0.1%到2.7%。通过这篇文章让我们了解其术后严重深部感染的相关治疗选择。
隆胸手术是最常见的美容整形手术,发生率从0.1%到2.7%。
在隆胸手术中,无论是否有植入物暴露,对于严重的深部组织植入物相关感染的最佳治疗方法尚无共识。传统上,通常的做法是先取出植入物,待感染控制后再植入新的植入物,这种方法可能会导致较差的美容结果和患者的满意度降低。此外,这两个阶段的手术可能会对患者产生重大的经济和心理影响。
因此,无论是通过抗生素积极的非手术治疗,还是通过一期取出植入物,保留植入物是一种有吸引力的选择。然而,在整形隆乳术后假体周围深部感染的病例中,单纯的抗生素治疗是一种不利的治疗方式,长期以来一直与较高的包膜挛缩率相关。通过这篇文章让我们了解相关治疗选择。
严重感染和隆乳手术中的植入物暴露是极具挑战性的并发症,可能导致长期的后遗症和治疗,并影响整形手术的美观效果。此外,根据环境的不同,这些并发症会带来巨大的经济成本,通常会给患者和外科医生带来负担。
排除轻度和浅表组织感染后,种植体相关感染的发生率为0.45%。在没有种植体暴露的情况下,非手术、基于抗生素的治疗显示出92.9%的治疗成功率。在植入物暴露的情况下,仅使用抗生素的治疗成功率下降到50%。这与以植入物为基础的乳房重建术的经验截然不同。更具体地说Spear和Seruya,以及Reish等人报告的严重感染或暴露种植体静脉注射抗生素治疗成功率为30.8%,植入物更换治疗成功率为37.3%。
因此,在存在种植体外露的情况下,建议立即手术入路。对于长时间感染(超过48小时)和表现出严重深部组织感染特征的患者,比如脓性引流并有假体外露,不推荐在隆胸整形术后一期保留假体。
文献来源:
Vasilakis V, Yamin F, Reish RG,Surgeons' Dilemma: Treatment of Implant-Associated Infection in the Cosmetic Breast Augmentation Patient.Aesthetic Plast Surg 2019 08;43(4)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#治疗方案#
78
#EST#
33
#AST#
40
#隆胸#
40
#植入物#
56
#植入#
35