European Radiology:利用深度学习和基于MRI的放射组学列线图自动预测骨肉瘤的新辅助化疗反应
2022-08-23 shaosai MedSci原创
放射组学从医学图像中提取定量的、可挖掘的、高维的数据,可以将放射图像与病变特征、治疗反应和病人预后联系起来,有助于回答与骨肉瘤患者实践密切相关的临床问题,并在NAC反应预测中显示出极高的临床前景。
众所周知,骨肉瘤是最常见的恶性原发性骨肿瘤,有两个发病高峰,一个是儿童和青少年,另一个是60岁以上的老年人。目前,这种肿瘤的治疗方法包括术前的新辅助化疗(NAC)以及结合手术和辅助化疗或放疗。然而,并非所有患者都能从目前的治疗策略中获益,尤其是那些对NAC没有病理良好反应(pGR)的患者来说更是如此。因此,影像学检查是术前预测骨肉瘤NAC反应的重要工具。
对肿瘤反应的预测通常是通过术前影像学检查对肿瘤体积、水肿、代谢指标等的变化进行估计。这些描述高度依赖专家的经验;因此,由于不可控的读者依赖因素,报告常会有很大差异。放射组学从医学图像中提取定量的、可挖掘的、高维的数据,可以将放射图像与病变特征、治疗反应和病人预后联系起来,有助于回答与骨肉瘤患者实践密切相关的临床问题,并在NAC反应预测中显示出极高的临床前景。
近日,发表在European Radiology杂志的一项研究探讨了从传统的术前磁共振序列中提取的放射组学特征在预测骨肉瘤患者对NAC反应方面的价值,比较了临床、放射组学和综合模型在区分pGRs和非pGRs方面的表现,并评估了这些放射组学特征在临床上的应用价值。
研究将144名接受NAC治疗的骨肉瘤患者被分为训练组(n = 101)和测试组(n = 43)。标准化后,使用nnU-Net训练的深度学习分割模型对术前MRI的ROI进行分割,并使用两个独立的人工分割作为标签。利用自动分割的ROI提取放射组学特征。在训练数据集中,通过五倍交叉验证进行特征选择。使用多种机器学习方法,用相同的训练数据集建立临床、放射组学和临床-放射组学模型,并用相同的测试数据集进行验证。分割模型是通过Dice系数来评估的。采用AUC和决策曲线分析(DCA)来说明模型性能和临床效用。
36/144(25.0%)名患者是对NAC的病理良好反应者(pGRs),而108/144(75.0%)名患者为非pGRs。在测试数据集上,分割模型的Dice系数达到了0.869。在测试数据集中,临床和放射组学模型的AUC达到0.636,95%的置信区间(CI)分别为0.427-0.860和0.759(95% CI,0.589-0.937)。临床放射学列线图显示出良好的辨别力,AUC为0.793(95% CI,0.610-0.975),准确率为79.1%。DCA表明了该列线图的临床效用。
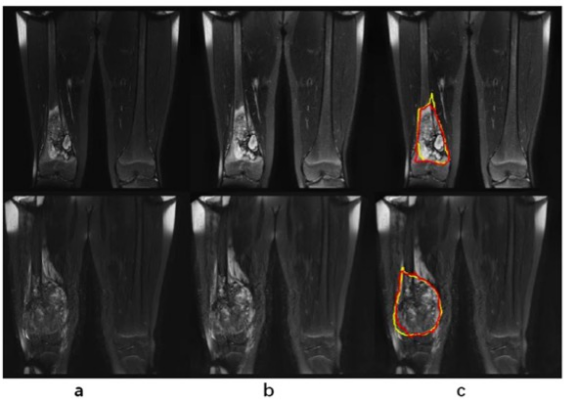
图 图像预处理和分割的结果。两行中显示的是两台不同扫描仪扫描的典型图像。在每一行中:a原始图像;b经CLAHE处理的图像;c经CLAHE处理的图像加上分割的结果(红色)和标签(黄色)
本研究研究建立了一个与基于MRI的自动化放射组学管道和客观临床变量相结合的列线图,可作为一个用于术前预测骨肉瘤患者病理NAC反应。的全自动影像学工具。
原文出处:
Jingyu Zhong,Chengxiu Zhang,Yangfan Hu,et al.Automated prediction of the neoadjuvant chemotherapy response in osteosarcoma with deep learning and an MRI-based radiomics nomogram.DOI:10.1007/s00330-022-08735-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#新辅助#
47
#PE#
31
#列线图#
44
#化疗反应#
42