AJRCCM:探索PET/CT对肺动脉高压炎症的评估
2021-10-27 刘少飞 MedSci原创
肺动脉高压是一组复杂的疾病,其特征是肺血管过度增殖性重塑,导致肺血管阻力增加、右心室 (RV) 过度后负荷,并最终增加右心室衰竭的风险和死亡。使用PET扫描将巨噬细胞募集到肺血管系统中来评估其炎症。


肺动脉高压(PAH)的临床特征是其症状和体征是非特异性的,这阻碍了早期诊断和及时治疗。目前的诊断工具,如右心导管插入术和超声心动图,无法可靠地识别早期 PAH 患者,要么是因为它们的侵入性太强而无法普遍使用,要么是因为它们不够准确。在 PAH 的几种病理生理机制中,PAH 患者的免疫过程改变和炎症未能解决的作用引起了广泛关注。在 PAH 的各种免疫效应细胞中,有多种证据表明巨噬细胞可能在 PAH 的发生和进展中起重要作用。具体而言,几项实验和临床研究一致表明,巨噬细胞浸润在 PAH 动物模型和 PAH 患者中尤为突出。已发现甘露糖受体 (MR) 阳性巨噬细胞的早期募集和激活对于 PAH 动物模型的开发至关重要,并且在特发性 PAH 患者的肺部中也会增加。总的来说,这些观察结果表明,肺部 MR 阳性巨噬细胞的分子成像可通过对肺部炎症状态进行成像来用于 PAH 的诊断和治疗监测。
本研究使用正电子发射断层扫描 (PET)/计算机断层扫描 (CT) 和一种靶向MR的示踪剂(简称:68Ga-NOTA-MSA),将巨噬细胞募集到肺血管系统中来准确评估 PAH,并且在动物 PAH 模型中测试了这一假设,并探索了 PAH 患者的转化潜力。
本研究首先对PAH大鼠的肺组织进行转录组学测序,在分析中发现与巨噬细胞相关的基因组显著富集。
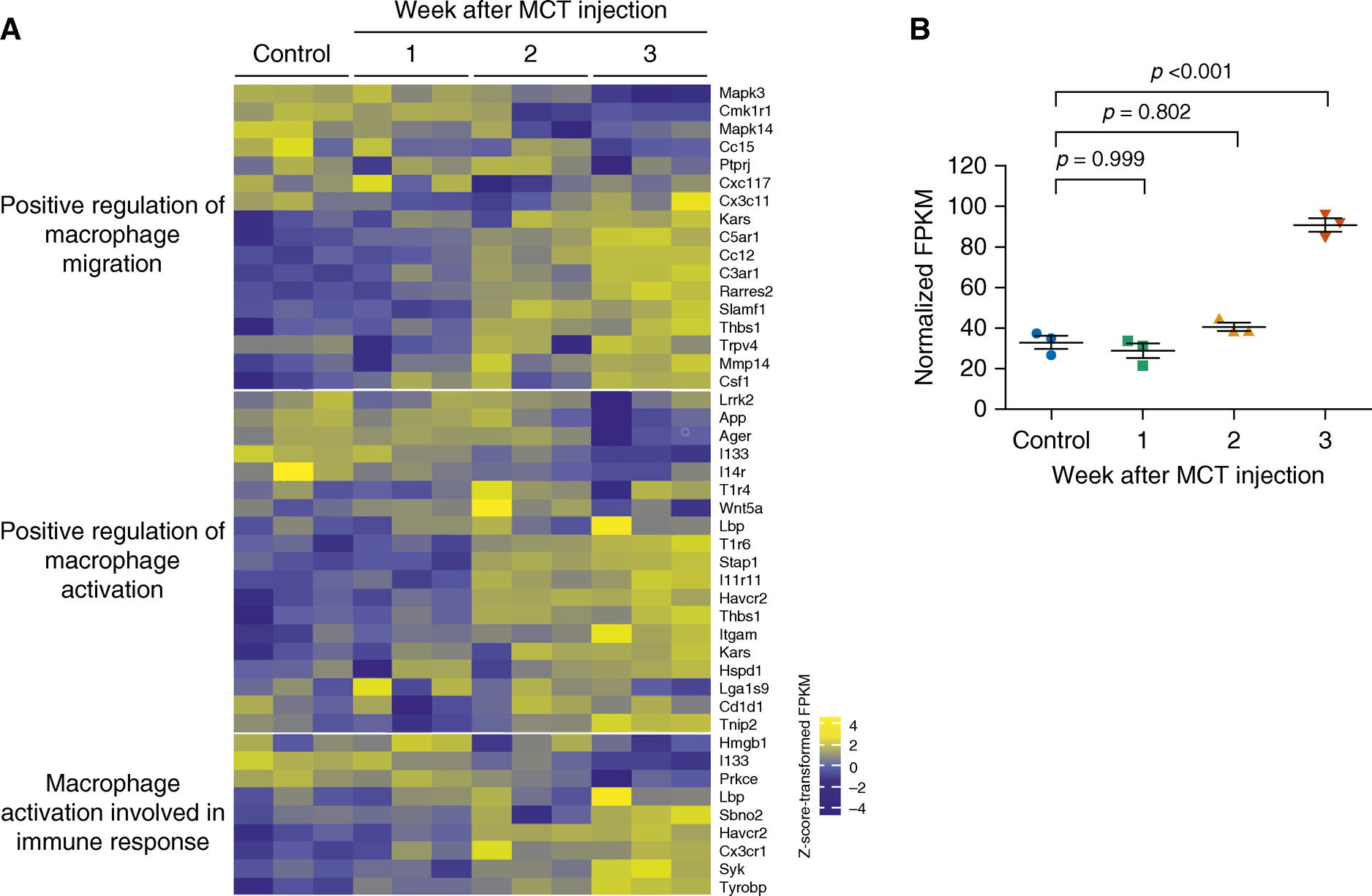
PAH 大鼠的连续 PET 图像表明,随着时间的推移,肺中 68Ga-NOTA-MSA 的吸收增加,这与免疫组织化学中观察到的 MR 阳性巨噬细胞募集相对应。
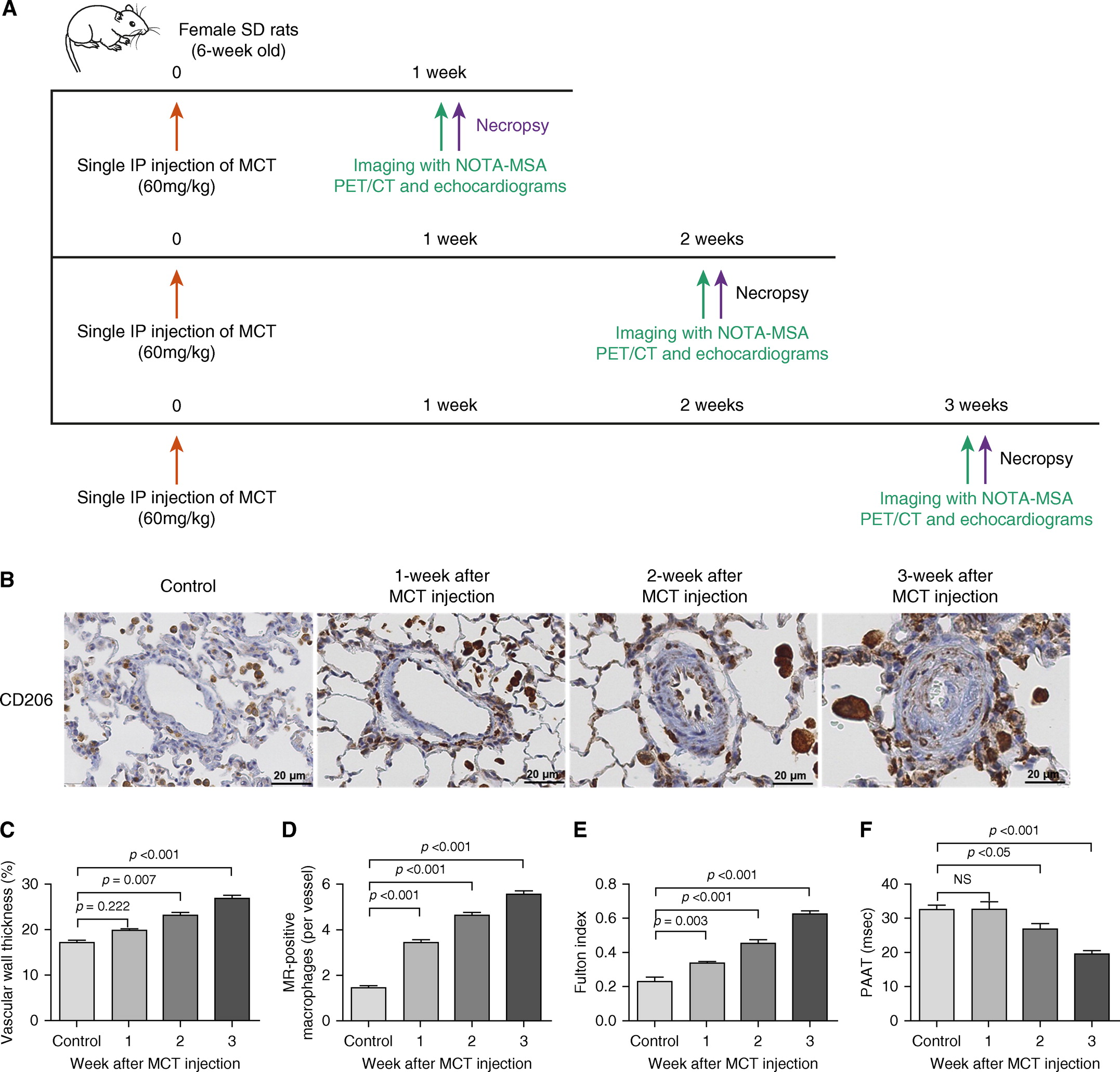
相比于西地那非或马西替坦治疗组的大鼠,MR 阳性巨噬细胞的组织学浸润和 68Ga-NOTA-MSA 在 PET 上的摄取显着低于对照组。

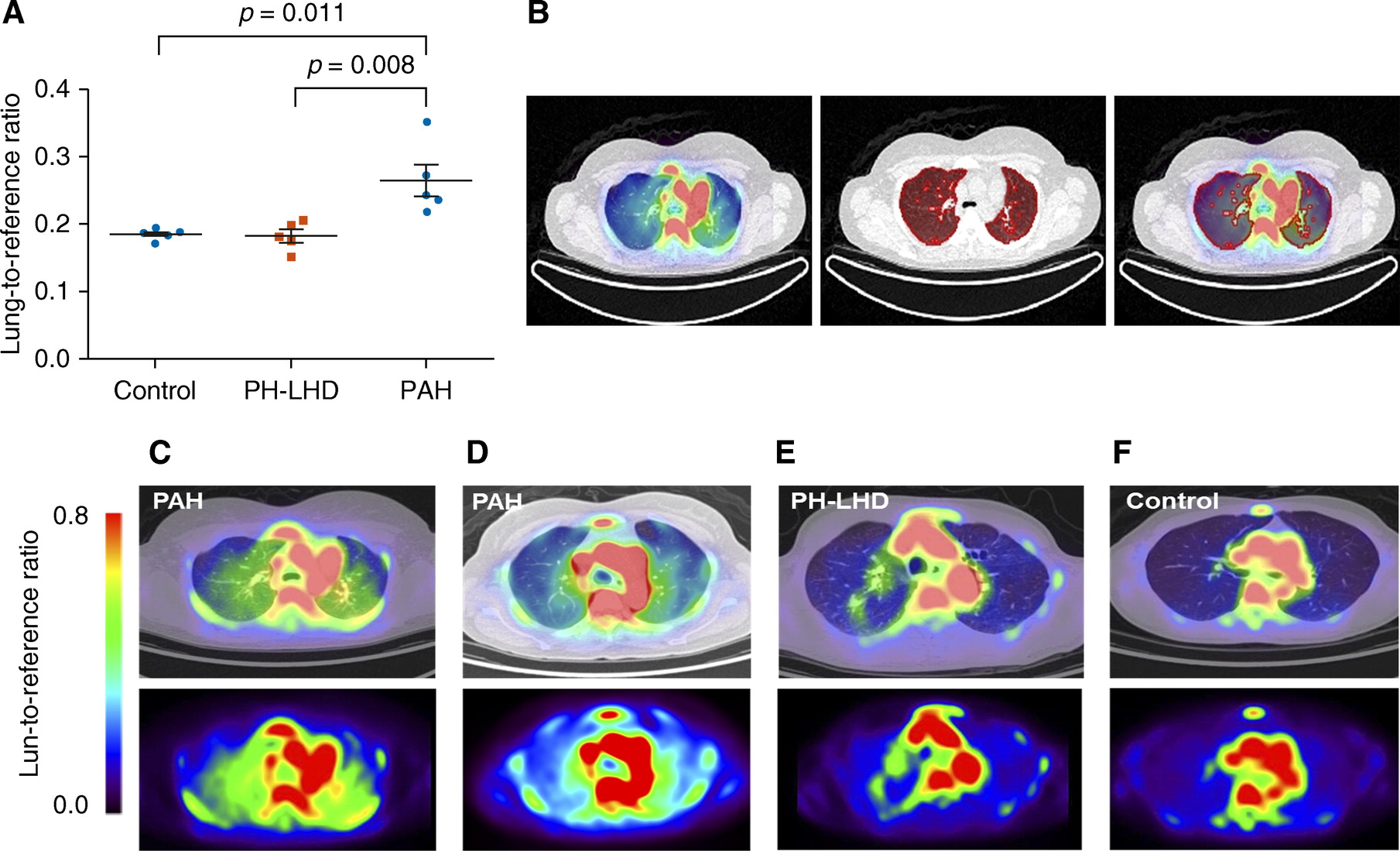
将该新思路运用到患者中,发现PAH 患者对 68Ga-NOTA-MSA 的肺摄取显着高于正常受试者 (P = 0.009) 或左心疾病导致的肺动脉高压患者 (P = 0.019)
这项研究为PAH的诊断和评估带来的启示是什么?
本研究假设巨噬细胞募集到肺血管系统可用于使用 68Ga-NOTA-MSA 正电子发射断层扫描 (PET) 评估 PAH,并在动物 PAH 模型和 PAH 患者中测试了这一假设。 68Ga-NOTA-MSA 在 PET 上的摄取增加发生在野百合碱注射后 1-3 周,这表明这种分子成像技术能够在血流动力学变化之前更早地检测到 PAH。 用西地那非或马西替坦治疗显着降低了肺 68Ga-NOTA-MSA 的摄取,支持该技术可能具有监测对 PAH 特异性治疗反应的潜在应用。 最后,PAH 患者的肺 68Ga-NOTA-MSA 摄取增加,但在正常受试者和左心疾病导致的肺动脉高压患者中均未增加,表明其具有转化潜力。
文章出处:
Park JB, Suh M, Park JY, Park JK, Kim YI, Kim H, Cho YS, Kang H, Kim K, Choi JH, Nam JW, Kim HK, Lee YS, Jeong JM, Kim YJ, Paeng JC, Lee SP. Assessment of Inflammation in Pulmonary Artery Hypertension by 68Ga-Mannosylated Human Serum Albumin. Am J Respir Crit Care Med. 2020 Jan 1;201(1):95-106. doi: 10.1164/rccm.201903-0639OC. PMID: 31322420.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
48
#RCC#
32
#动脉高压#
39
#PET/CT#
68
#PET#
42