J Dent Res:反应性牙本质形成的调控
2017-12-02 lishiting MedSci原创
在治疗未累及牙髓的龋齿过程中,尽可能多的保存未受影响的牙本质是在物理性移除腐败矿化物过程中的一个主要目标。牙本质的损伤会引起牙本质内促矿化因子的释放 (转移生长因子-β [TGF-β]和骨形成蛋白[BMP]),它被认为可以刺激成牙本质细胞分泌形成新的“第三期”牙本质(反应性牙本质)。反应性牙本质是在牙髓表面形成的牙本质,它可以增加牙本质的厚度。作者之前的研究发现,Wnt/β-catenin信号的激
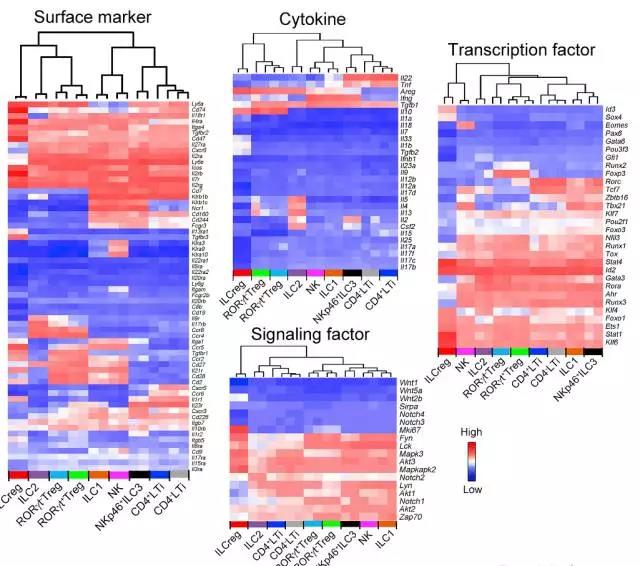
在治疗未累及牙髓的龋齿过程中,尽可能多的保存未受影响的牙本质是在物理性移除腐败矿化物过程中的一个主要目标。牙本质的损伤会引起牙本质内促矿化因子的释放 (转移生长因子-β [TGF-β]和骨形成蛋白[BMP]),它被认为可以刺激成牙本质细胞分泌形成新的"第三期"牙本质(反应性牙本质)。反应性牙本质是在牙髓表面形成的牙本质,它可以增加牙本质的厚度。作者之前的研究发现,Wnt/β-catenin信号的激活对于暴露的牙髓损伤的牙齿修复起到至关重要的作用,并且该通路可以被小分子GSK-3拮抗剂所激活,进而增强修复性牙本质的形成。在此,研究者通过未暴露的牙髓损伤模型并采用小分子调节Wnt/β-catenin, TGF-β和BMP通路的方法来探讨体内反应性牙本质形成的机制。结果显示,在损伤部位局部增强Wnt信号活性会加强反应性牙本质的分泌。另外,抑制TGF-β, BMP或Wnt通路并没有阻碍反应性牙本质的形成,尽管抑制TGF-β或/和BMP信号会导致更多的紊乱、无小管的牙本质形成。结果表明,Wnt/β-catenin信号对反应性牙本质的形成并未起到至关重要的作用,但是对于修复性牙本质的形成,外源性的
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#反应性#
33
好好好好好好好好
67
#牙本质#
47
学习
55
TGF-β或BMPs信号
47