JACC:经导管主动脉瓣置换术后的再次手术
2020-07-23 xiangting MedSci原创
与一开始就接受SAVR的患者相比,TAVR早期失败后再进行SAVR虽然少见,但预后不良。
这项研究使用胸外科医师协会(STS)成人心脏手术数据库,报道了经导管主动脉瓣置换术(TAVR)后再次进行外科手术的最大患者系列。
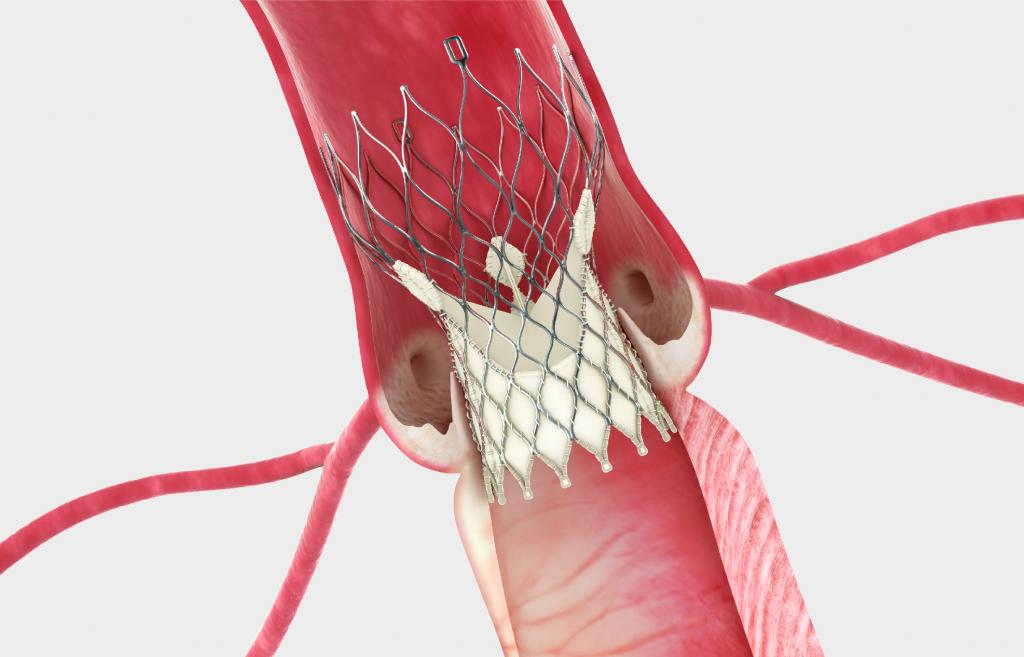
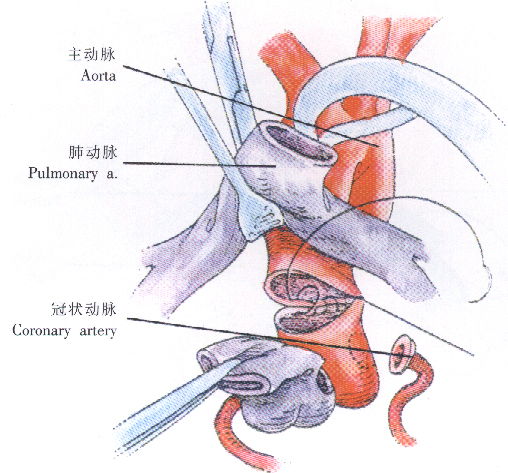
TAVR已成为治疗主动脉瓣狭窄的有效手段。随着TAVR逐渐被用于低风险人群,装置失效的治疗变得越来越重要。
在STS成人心脏手术数据库中查找2011年至2015年接受外科主动脉瓣置换并有TAVR史的患者。确定实际/预期(O/E)死亡率比值,以方便对不同手术指征和TAVR手术后时间进行比较。
共有123名患者符合入选标准(中位年龄77岁),分别有17%、24%和59%的患者STS预测死亡风险为 4%、4%-8%和>8%。再次手术的中位时间为2.5个月(四分位范围:0.7-13.0),手术死亡率为17.1%。再次手术的常见指征包括早期TAVR装置失效,如瓣周漏(15%)、结构性瓣膜退化(11%)、修复失败(11%)、尺寸或位置问题(11%)和瓣膜性心内膜炎(10%)。所有的术前风险类别均与O/E死亡率比值升高相关(预测死亡风险<4%:O/E 5.5;4%-8%:O/E 1.7;>8%:O/E 1.2) 。
与一开始就接受SAVR的患者相比,TAVR早期失败后再进行SAVR虽然少见,但预后不良。对于这种不断发展的技术,需要继续积累经验以减少早期TAVR失败的发生率,并进一步确定TAVR瓣膜失效的最佳治疗方法。
原始出处:
Oliver K. Jawitz. Reoperation After Transcatheter Aortic Valve Replacement An Analysis of the Society of Thoracic Surgeons Database. JACC:Cardiovascular Interventions. July 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
32
学习了
76
#置换#
29
学习一下
101
#ACC#
35
#主动脉瓣#
29
#主动脉瓣置换术#
38
#主动脉#
29
#经导管#
37
#经导管主动脉瓣置换#
29