Cell Reports:CDK抑制剂与免疫疗法强强联手,复发性乳腺癌有救了
2021-05-15 生物探索 生物探索
新研究发现细胞周期蛋白依赖性激酶(CDK)抑制剂可显著改善复发性乳腺癌的免疫治疗效果。
癌症的免疫治疗是近些年新兴的一种治疗手段,不仅革命性地改变了癌症治疗的效果,而且还革命性地改变了治疗癌症的理念。然而,由于晚期乳腺肿瘤中的杀伤性T淋巴细胞数量很少,因此免疫疗法效果往往不尽如意。

近日,俄亥俄州立大学综合癌症中心的科研人员在《Cell Reports》杂志发表了一篇题为Metabolic modulation by CDK4/6 inhibitor promotes chemokine-mediated recruitment of T cells into mammary tumors的新研究报告,发现细胞周期蛋白依赖性激酶(CDK)抑制剂可显着改善复发性乳腺癌的免疫治疗效果。
为了探究CDK4/6抑制剂帕博西尼(PALBOCICLIB)对肿瘤免疫微环境的影响,研究人员分别利用乳腺癌 MMTV-PyMT 转基因小鼠(FVB小鼠)和接种PYMT肿瘤细胞的雌性C57BL / 6小鼠进行分析,以确定不同模型(自发与移植)和遗传背景下CDK4/6抑制剂的药效是否一致。
在此基础上,研究人员基于流式细胞仪分析了CDK4 / 6对肿瘤免疫微环境组成的影响,与此同时,利用光谱细胞仪表征了CDK4 / 6对肿瘤浸润T细胞表型的影响。研究发现,CDK4/6抑制剂可增加乳腺癌小鼠模型中肿瘤T细胞的数量和活性。
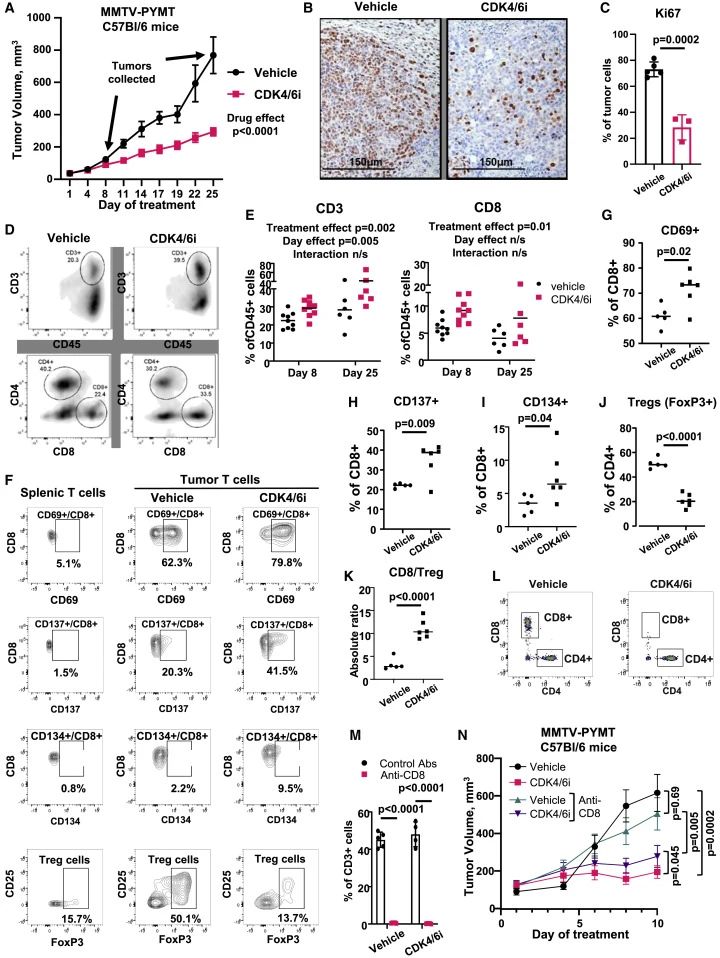
CDK4 / 6治疗增加了乳腺癌小鼠模型中T细胞的数量和活性
基于以上研究,研究人员猜测CDK4 / 6抑制剂激活T细胞水平的能力或许可应用于癌症免疫疗法中。
与预期一致,研究发现,与仅使用CDK4 / 6抑制剂治疗的小鼠相比,接种PYMT细胞的小鼠经OX40激动剂和4-1BB激动剂刺激,再经CDK4 / 6抑制剂治疗后能使趋化因子“吸引”T细胞侵入肿瘤,从而更有效的抑制肿瘤的生长。
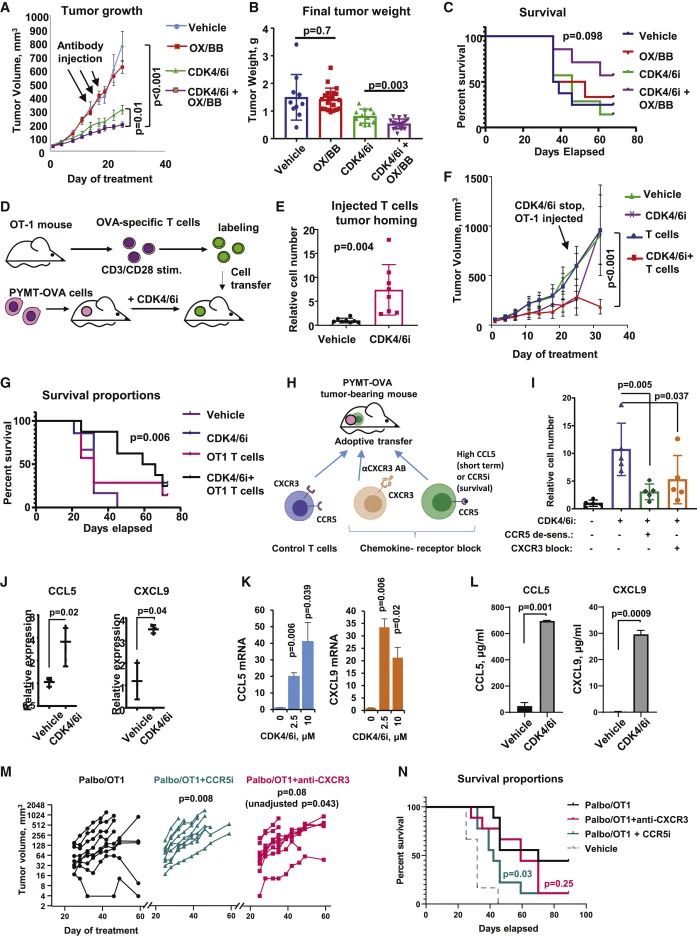
CDK4 / 6改善免疫治疗反应并促进趋化因子介导的T细胞肿瘤归巢
早前有研究表明,mTOR信号通路在某些免疫细胞亚群中会诱导趋化因子,且在CDK4 / 6抑制剂的治疗背景下靶向PI3K / mTOR途径可改善肿瘤的生长抑制作用,同时防止肿瘤通过内在机制获得耐药性。
但由于以往的试验使用的都是免疫缺陷小鼠。因此,研究人员在这项最新的研究中测试了CDK4 / 6和mTOR联合抑制如何影响免疫正常小鼠的肿瘤生长和免疫浸润。研究发现,在CDK4 / 6i和mTORi联合治疗组中,肿瘤的生长受到明显的抑制。
接下来,研究人员试图确定mTOR到底如何调节CDK4 / 6i处理的细胞的趋化因子表达?
众所周知,mTOR信号通路是细胞代谢的中央调节剂,而葡萄糖和谷氨酰胺是癌细胞生长所需的关键营养素,其消耗量反映了细胞的代谢需求。
因此,研究人员通过检测经CDK4 / 6处理的MCF7细胞中的葡萄糖摄取率与谷氨酰胺的利用情况,进一步分析了CDK4 / 6处理的细胞是否具有代谢活性。研究发现,需要mTOR信号通路来维持CDK4 / 6处理后的细胞的代谢活性。
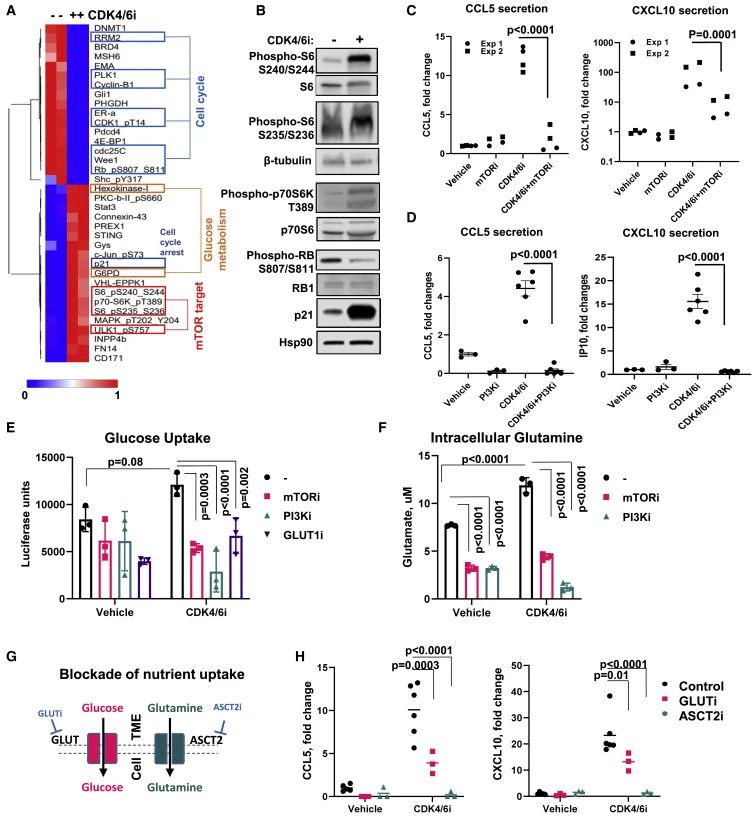
CDK4 / 6介导的趋化因子诱导需要mTOR调节的代谢活性
总而言之,该研究表明,CDK4 / 6抑制剂可提供一种将T细胞吸引到乳腺肿瘤中的治疗新策略,从而增加免疫疗法的敏感性。期待这项新研究能提高乳腺癌的生存期,给晚期乳腺癌一线治疗带来突破性进展。
原始出处:
Roman V. Uzhachenko, et al. Metabolic modulation by CDK4/6 inhibitor promotes chemokine-mediated recruitment of T cells into mammary tumors. Cell reportes, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CEL#
20
#复发性#
24
#Cell#
33
#抑制剂#
27
#CDK#
34