Immunity:清华大学医学院祁海课题组揭示滤泡辅助性T细胞和体液免疫反应调控新机制
2018-08-06 佚名 清华免疫
2018年7月31日,《Immunity》杂志以长文形式在线发表了清华大学免疫学研究所祁海教授课题组题为《PD-1 controls follicular T helper cell positioning and function》的研究论文。该论文深入研究了经典共抑制分子PD-1如何调控T细胞被招募迁移进入滤泡区,帮助B细胞建立生发中心反应,并产生高亲和力抗体的分子机制,为未来疫苗研发和免疫治
2018年7月31日,《Immunity》杂志以长文形式在线发表了清华大学免疫学研究所祁海教授课题组题为《PD-1 controls follicular T helper cell positioning and function》的研究论文。该论文深入研究了经典共抑制分子PD-1如何调控T细胞被招募迁移进入滤泡区,帮助B细胞建立生发中心反应,并产生高亲和力抗体的分子机制,为未来疫苗研发和免疫治疗提供了潜在新思路。PTN项目毕业生史静雯博士为该论文的第一作者,侯诗玥博士、刘欣博士和CLS博士生方谦也做出了重要贡献。
在机体遭遇外来病原体感染时,原本定居于淋巴组织T细胞区的抗原特异性CD4+ T细胞可以在活化后迁移至B细胞滤泡区,并帮助B细胞建立生发中心。在生发中心,B细胞在大量增殖的同时伴随体细胞高频突变,通过亲和力筛选产生高亲和力抗体和长效体液免疫。这类定位于滤泡区的CD4+ T细胞亚群被称作滤泡辅助性T细胞(follicular helper T cell,TFH),它们是体液免疫的重要调控细胞亚群,也是近年细胞免疫学的研究热点之一。
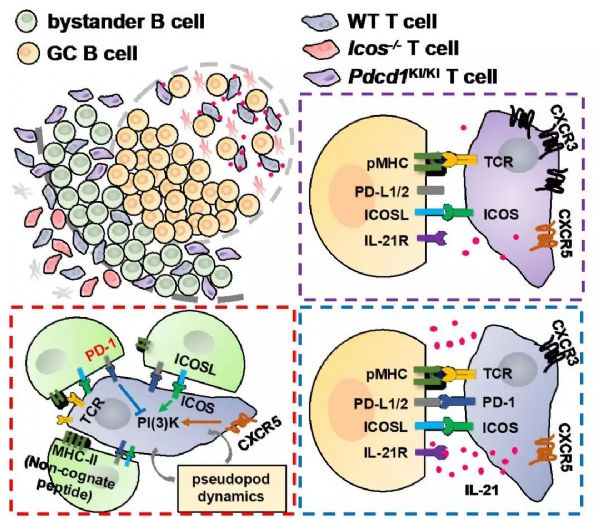
T细胞招募进入滤泡区的过程依赖能响应滤泡区趋化因子的CXCR5受体和共刺激分子ICOS。祁海课题组2013年发表于《Nature》的工作显示,ICOS介导的T细胞运动依赖于PI3K通路的活性和滤泡区抗原非特异性初始B细胞上持续表达的ICOSL。然而,ICOS在T细胞区域并不调控T细胞运动,暗示了滤泡区微环境可能为T细胞深入迁移设置了某种障碍。在本论文中,作者发现TFH细胞标志分子PD-1是参与抑制T细胞招募进入滤泡区的关键信号分子,并且这种抑制来源于滤泡区幼稚B细胞上持续高表达的配体PD-L1。PD-1受体接受刺激时即可抑制CXCR5或ICOS诱导的PI3K活性, 而这一抑制作用不需要TCR信号,被称为抗原非依赖的旁观工作模式。而PD-1过表达的T细胞在体内显示出向滤泡区归巢的缺陷。通过利用T细胞活化后无法上调PD-1表达的基因工程小鼠,作者进一步证明抑制PD-1上调就可以拯救ICOS信号缺失下T细胞无法进入滤泡区的缺陷。这些结果解释了在TFH形成的过程中,为什么会在T-B交界区开始需要ICOS信号来促进PI3K活化而帮助T细胞迁移进入滤泡区。
作者还进一步探究了PD-1对TFH细胞的功能调控,发现PD-1信号虽然对T细胞招募进入滤泡区起抑制作用,但却可以帮助已经进入滤泡区的TFH细胞集中于需要它们发挥功能的生发中心区域。这一方面是因为GC B细胞相对于幼稚B细胞下调了PD-L1的表达,而高表达PD-1的TFH细胞更易于留在配体低表达的GC区域;另一方面是PD-1共抑制信号限制了T细胞活化过程中趋化因子CXCR3的表达,从而使TFH细胞免受到滤泡区外围CXCL9和CXCL10的趋化吸引作用。在生发中心内部,无论当TFH细胞无法上调PD-1还是B细胞上缺失PD-L1,都会导致GC B细胞数量增加,但亲和力下降,说明PD-L1-PD-1信号是生发中心亲和力筛选的保证因素之一。因此,以抗原非依赖的旁观模式或者共刺激模式的两种方式,通过对TFH分化、迁移、和功能的一系列精密调控,TFH细胞上的PD-1受体对生发中心反应幅度与效率起了至关重要的作用。
祁海课题组的这一工作和先前有关ICOS的工作完整描绘了TFH细胞招募过程,新颖地揭示了一向被忽视的抗原非特异性幼稚B细胞的重要功能和经典共刺激分子ICOS和PD-1在无TCR信号下的旁观工作模式,为未来改进疫苗研发提供了新思路,对其它炎症或癌症组织中T细胞招募研究也有启示作用。中国科学院上海生物化学与细胞生物学研究所刘小龙教授团队对该项目完成提供了重要帮助。该研究项目得到了科技部973计划,国家自然科学基金委杰出青年基金、重点项目、创新群体项目的支持,并得到盖茨基金会和美国HHMI国际学者项目的资助。
原始出处:Jingwen Shi, Shiyue Hou, Qian Fang, et al. PD-1 Controls Follicular T Helper Cell Positioning and Function. Immunity. 2018 Jul 16.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#医学院#
37
#辅助性T细胞#
34
#体液免疫反应#
28
#Immunity#
29
#免疫反应#
0
#清华#
32