Eur Urol Oncol:68 Ga-前列腺特异性膜抗原正电子发射断层扫描/计算机断层扫描和多参数磁共振成像在预测前列腺活检病理方面的联合效用
2021-03-31 AlexYang MedSci原创
68镓标记的前列腺特异性膜抗原正电子发射断层扫描(68Ga-PSMA-11 PET)是一种有价值的分期工具,但其在表征原发性前列腺癌方面的效用仍不清楚。最大标准化摄取值(SUVmax)是PET无损伤病
68镓标记的前列腺特异性膜抗原正电子发射断层扫描(68Ga-PSMA-11 PET)是一种有价值的分期工具,但其在表征原发性前列腺癌方面的效用仍不清楚。最大标准化摄取值(SUVmax)是PET无损伤病灶内最高放射性示踪剂摄取量的量化测量。

最近,有研究人员评估了SUVmax在单独活检和联合多参数磁共振成像(mpMRI)中检测临床显著性前列腺癌(csPCa)的效用。
研究人员对2016年至2018年期间接受68Ga-PSMA-11 PET/CT、mpMRI和经尿道模板前列腺活检的200名男性进行了回顾性分析。研究结果表明,GG 3-5肿瘤的中位SUVmax(6.40,四分位数范围[IQR]4.47-11.0)大于良性和GG 1-2肿瘤(3.14,IQR 2.55-3.91;P<0.001)。GG 3的中位SUVmax(5.70,IQR 3.68-8.67)大于GG 2的中位SUVmax(3.47,IQR 2.70-4.74;P<0.001)。对于GG 3-5疾病,敏感性分别为86.5%、95.9%和98.6%,阴性预测值(NPV)分别为88.4%、88.5%和93.3% (SUVmax≥4,PI-RADS评分为3-5)。该组合模型比单独使用mpMRI检测到更多的GG 3-5疾病(98.6% vs 95.9%;p=0.04)。SUVmax是GG 3-5疾病的csPCa的独立预测因子(单位OR 1.27,95%CI 1.13-1.45)。他们的结果受到回顾性研究设计的限制。
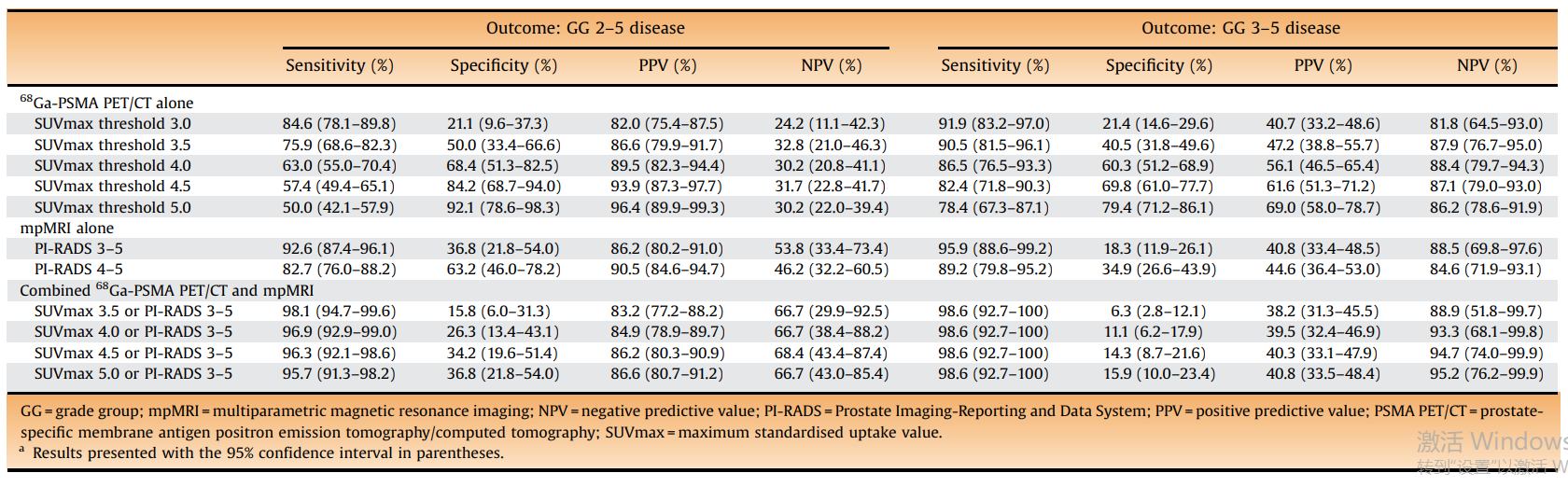
最后,研究人员指出,68Ga-PSMA-11 PET/CT中更大的SUVmax与活检发现GG 3-5癌有关。PI-RADS评分和SUVmax的联用比单独使用任何一种都具有更高的敏感性和NPV。68Ga-PSMA-11 PET/CT与mpMRI联用可能对改善局部疾病的风险分层是有用的。
原始出处:
Arveen A Kalapara, Zita E Ballok , Shakher Ramdave et al. Combined Utility of 68 Ga-Prostate-specific Membrane Antigen Positron Emission Tomography/Computed Tomography and Multiparametric Magnetic Resonance Imaging in Predicting Prostate Biopsy Pathology. Eur Urol Oncol. Mar 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oncol#
57
#前列腺特异性膜抗原#
52
#前列腺活检#
39
#特异性#
50
#计算机#
54
#活检#
36
#磁共振#
26
#抗原#
39
学习啦
78
谢谢梅斯分享这么多精彩信息
56