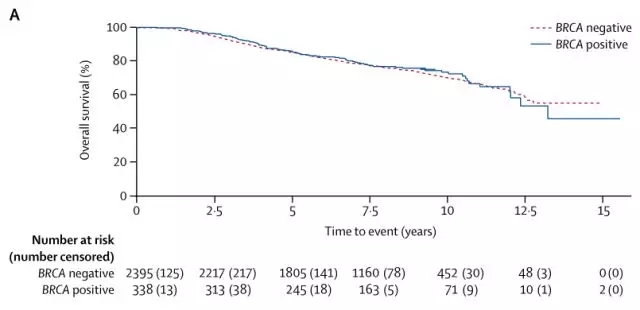
Lancet Oncol:BRCA突变并不影响乳腺癌患者生存率!双乳切除未必真的获益!并不影响乳腺癌患者生存率!双乳切除未必真的获益!
2018-01-16 Juka 转化医学网
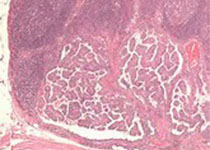
美国著名影星安吉丽娜·朱莉在颠覆的时刻选择了切掉自己的乳房,因为她的祖传基因里面埋藏着乳腺癌的种子。这一举动于安吉丽娜·朱莉而言,是极其需要勇气的行为,这也使得肿瘤基因检测得到极大的推广。然而在《Lancet》的一项大型研究却发现:乳腺癌基因并不会增加患者死亡率!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#患者生存#
25
#Oncol#
34
#Lancet#
32
#生存率#
26
#BRCA突变#
34
#乳腺癌患者#
28
#BRCA#
34
henhao
65
谢谢分享.
50
继续关注.
62