Chest:间质性肺疾病患者肺动脉高压的筛查策略
2022-02-19 刘少飞 MedSci原创
许多间质性肺病 (ILD) 患者可能会从早期评估肺动脉高压 (PH) 中受益,因为已经有批准的治疗方法可用。评估 ILD 患者的方案通常与评估 PH-ILD 重叠,可用于评估 PH 的风险。
研究背景:
肺动脉高压 (PH) 是间质性肺病 (ILD) 的常见并发症,并与较差的结果和增加的死亡率相关。建议在肺移植候选者中评估 PH,但目前没有标准化的筛选方法。最近的试验已经确定了在这种情况下有效的治疗方法,为常规筛查 ILD 患者的 PH 提供了另一个基本原理。研究问题专家共识支持哪些筛查策略来识别 ILD 患者的 PH?
研究设计和方法:
该研究召集了一个由 16 名在 PH 和 ILD 方面具有专业知识的肺病专家组成的小组,并利用经过修改的 Delphi 共识流程和 3 次调查来确定 PH 筛查策略。调查 1 主要由开放式问题组成。调查 2 和 3 是根据对调查 1 的答复制定的,其中包含有关 PH 筛查的陈述,小组成员从 -5(非常不同意)到 +5(非常同意)评级。
研究结果:
小组成员就怀疑 PH 的几个触发因素达成共识,包括:症状、临床体征、胸部计算机断层扫描或其他影像学检查结果、脉搏血氧饱和度异常、脑利钠肽 (BNP) 或 N 末端前肽 (NT-proBNP) 升高,在肺功能测试或 6 分钟步行距离中出现无法解释的恶化。超声心动图和 BNP/NT-proBNP 被确定为 PH 的筛查工具。右心导管插入术被认为是确认 PH 的必要条件。
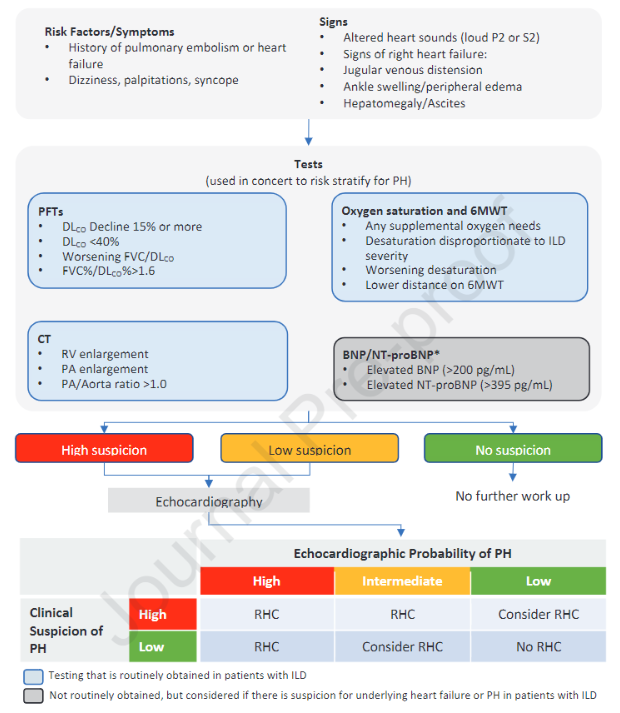
研究启示:许多 ILD 患者可能会从早期评估 PH 中受益,因为已经有批准的治疗方法可用。评估 ILD 患者的方案通常与评估 PH-ILD 重叠,可用于评估 PH 的风险。由于缺乏标准化方法,本共识声明旨在帮助临床医生识别 ILD 和可能的 PH 患者,并为及时进行右心导管插入术提供指导。
参考文献:
Rahaghi FF. Screening Strategies for Pulmonary Hypertension in Patients with Interstitial Lung Disease: A Multidisciplinary Delphi Study. Chest. 2022 Feb 14:S0012-3692(22)00262-8. doi: 10.1016/j.chest.2022.02.012. Epub ahead of print. PMID: 35176276.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Chest#
52
#EST#
36
#动脉高压#
41
#疾病患者#
27
#间质性#
41
#筛查##间质性肺病#
95
#间质性肺疾病#
29