Nature子刊:浙大易文/周如鸿合作揭示糖基化调控胰腺癌新机制
2022-07-28 生物世界 生物世界
胰腺癌是一种恶性程度极高的消化系统肿瘤,确诊后患者的五年生存率仅为10%左右。代谢的改变是肿瘤细胞的重要特征之一。肿瘤细胞通过代谢重编程产生其快速增殖所需的物质、能量以及氧化还原力。
胰腺癌是一种恶性程度极高的消化系统肿瘤,确诊后患者的五年生存率仅为10%左右。代谢的改变是肿瘤细胞的重要特征之一。肿瘤细胞通过代谢重编程产生其快速增殖所需的物质、能量以及氧化还原力。癌基因Kras突变的胰腺导管腺癌(PDAC,胰腺癌中最常见的病理类型)的增殖高度依赖谷氨酰胺(Gln)分解代谢途径。在该途径中,Gln首先被转化成天冬氨酸(Asp),随后在谷草转氨酶(GOT1)催化下形成草酰乙酸(OAA),OAA经苹果酸脱氢酶(MDH1)催化进一步被转化为苹果酸(Malate),再经苹果酸酶(ME1)氧化最终形成丙酮酸(Pyruvate)和NADPH;后者能提供还原当量,维持细胞内氧化还原平衡。该途径对于PDAC细胞的增殖和存活至关重要,因此深入了解这一途径的调控机制有助于为PDAC的临床治疗提供新的思路和靶点。
O-GlcNAc糖基化修饰是通过N-乙酰葡糖胺以β-糖苷键形式共价连接到蛋白质的丝氨酸(Ser)或苏氨酸(Thr)羟基上的一种翻译后修饰。该修饰是一种高度动态的修饰方式,会随着细胞内的营养状态和细胞外的刺激发生变化。该修饰广泛发生在细胞内的蛋白上,并调控基因转录、信号传导、蛋白合成和代谢重编程等重要的生物学过程。之前的研究表明O-GlcNAc糖基化修饰水平在PDAC中异常增高。然而O-GlcNAc糖基化调控PDAC发生发展的分子机制尚不清楚。
2022年7月25日,浙江大学生命科学学院易文教授课题组和周如鸿教授课题组合作在 Nature Chemical Biology 杂期刊在线发表了题为:O-GlcNAcylation promotes pancreatic tumor growth by regulating malate dehydrogenase 1 的研究论文。
该研究通过糖化学生物学、肿瘤生物学和计算生物学多学科交叉手段,揭示了O-GlcNAc糖基化调控谷氨酰胺代谢,促进PDAC生长的分子机制。
研究首先发现介导O-GlcNAc修饰的糖基转移酶OGT的表达在胰腺癌病人组织中显著升高;敲低OGT显著抑制了PDAC细胞的Gln代谢,抑制了PDAC细胞增殖。
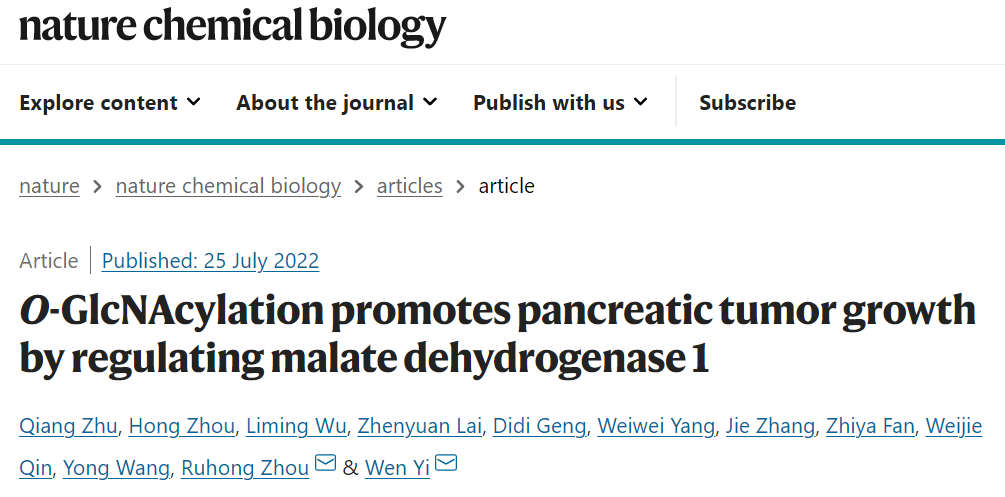
进一步研究发现O-GlcNAc修饰对Gln代谢途径中的关键酶MDH1的功能有显著影响。通过高分辨质谱结合点突变的方法鉴定出Ser189位为MDH1的糖基化修饰位点。体外的酶活实验表明Ser189位上的糖基化可以增强其酶活性。靶向代谢组学实验证实了MDH1糖基化促进Gln代谢和NADPH的产生。
此外,MDH1参与细胞内协调糖酵解和线粒体呼吸作用的苹果酸-天冬氨酸穿梭途径;MDH1糖基化会有利于NADH的再生,从而促进的线粒体的呼吸。小鼠体内成瘤实验和临床样本分析也进一步验证了MDH1 Ser189位的糖基化修饰对PDAC生长的促进作用。
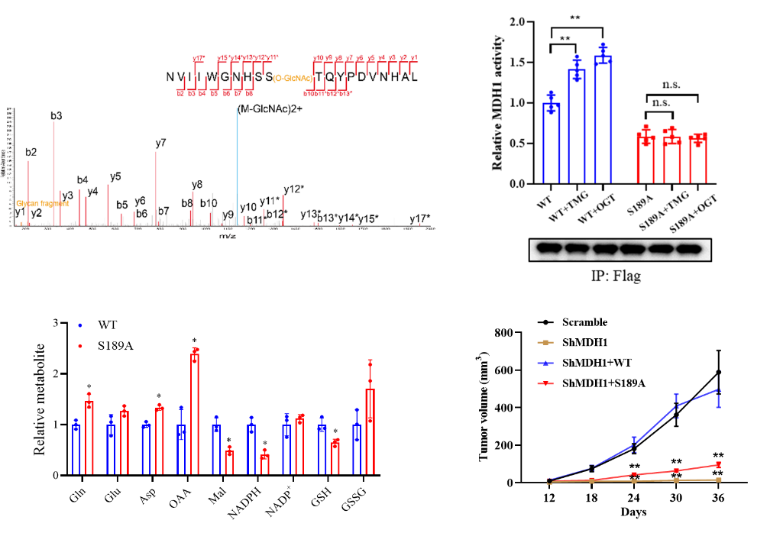
图1:MDH1 Ser189位的糖基化修饰促进了其酶活以及PDAC生长
为了进一步了解O-GlcNAc糖基化增强MDH1酶活性的分子机制,作者利用全原子分子动力学模拟对MDH1单体-底物(NADH,MAK)复合物在Ser189糖基化和非糖基化状态下的动力学行为进行了探究。结果表明底物在糖基化情况下更加稳定,结合概率更高。这得益于Ser189 O-GlcNAc对底物结合口袋的保护,促使MDH1与底物,底物与底物之间相互作用增强;MDH1和底物之间增强的相互作用主要来自Ser189 O-GlcNAc与蛋白残基Gln228、Gln229和Arg98的接触贡献。相应的三联体突变(Q228A/Q229A/R98A)活性分析实验也证实了这一观察结果。
此外,与单体不同,MDH1二聚体在非糖基化和糖基化状态下的底物结合并没有表现出显著差异。这可能是由于参与底物结合口袋的螺旋区域受到了二聚体界面相互作用的约束,不似单体中那样灵活。总的来说,Ser189 O-GlcNAc可以充当“分子胶”的作用,通过稳定MDH1单体上的底物结合口袋,增强蛋白与底物,底物与底物之间的相互作用,来提高底物的结合及稳定性,最终促进MDH1的酶活性。
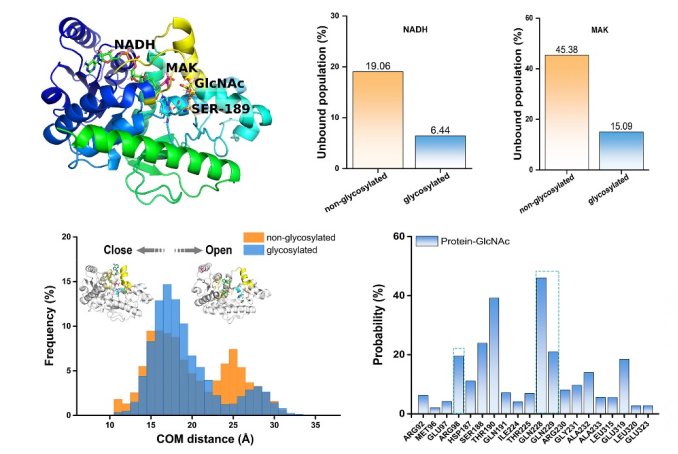
图2:MDH1 Ser189位上的O-GlcNAc糖基化促进其酶活性的分子机理
综上所述,该研究揭示了OGT-MDH1轴在PDAC发生和发展过程中的重要功能。鉴于MDH1在PDAC中高表达,且MDH1糖基化水平与PDAC进程呈正相关,该研究成果提示干预MDH1糖基化可以作为靶向PDAC的潜在策略。
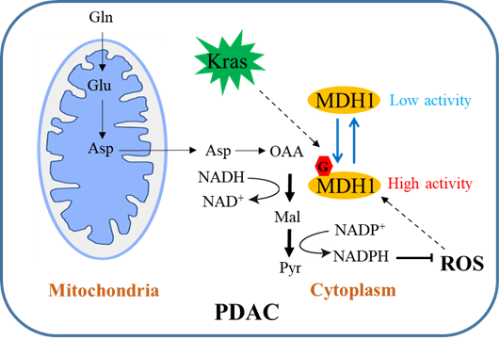
图3:MDH1糖基化调控PDAC生长的工作模式图
教育部“生命系统稳态与保护”重点实验室、浙江大学生命科学学院、浙江大学上海高等研究院、浙江大学癌症研究院周如鸿教授和易文教授为论文的共同通讯作者。浙江大学生命科学学院博士后朱强和周红为论文的共同第一作者,王勇研究员也参与了这项工作。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
0
#糖基化#
52
#浙大#
0
收藏
44