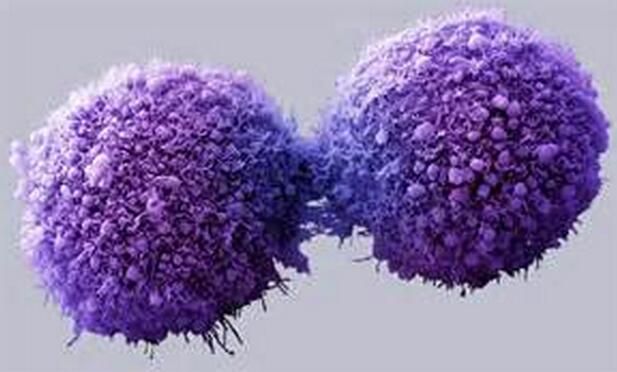
Cancer Cell:为何癌症儿童深受放化疗毒害?
2017-01-09 佚名 生物谷
尽管近年来儿科肿瘤治疗取得了一些进展,但是化疗及放疗经常给这些年轻的孩子的脑、心及其他重要器官带来持久而严重的损伤,但是成年人的这些器官相对安全。这种差别迄今为止都没有得到合理的解释,这就导致医生需要平衡用药——他们需要给患儿使用足够高的剂量以杀死肿瘤细胞,同时又不能太高以至于带来严重副作用,但是由于重要器官还比较脆弱,婴儿和儿童的这个剂量范围非常窄。 如今,达纳法博癌症中心的科学家宣布他

尽管近年来儿科肿瘤治疗取得了一些进展,但是化疗及放疗经常给这些年轻的孩子的脑、心及其他重要器官带来持久而严重的损伤,但是成年人的这些器官相对安全。这种差别迄今为止都没有得到合理的解释,这就导致医生需要平衡用药——他们需要给患儿使用足够高的剂量以杀死肿瘤细胞,同时又不能太高以至于带来严重副作用,但是由于重要器官还比较脆弱,婴儿和儿童的这个剂量范围非常窄。
如今,达纳法博癌症中心的科学家宣布他们已经发现了一个可能解释儿童的器官更容易受损的原因,相关成果发表在《Cancer Cell》上。在这项新研究中,他们发现尚处于发育中的器官在遭受化疗或者放疗的毒性压力下更容易发生凋亡。
“凋亡是一种使细胞自己死亡的分子信号,它在决定发育细胞的命运(即细胞的最终形式及功能)中发挥重要作用。例如凋亡可以帮助清除大脑中不需要的细胞间连接,但是在发育早期大脑中比较活跃的凋亡信号也使大脑对任何损伤或压力比较敏感。”研究论文的第一作者Kristopher A. Sarosiek博士如是说,他是哈佛T.H. Chan公共卫生学院放射生物学副教授。
化疗、放疗及其它治疗方式通常使肿瘤细胞通过凋亡而死亡,尽管它们可以通过激活生存前信号避免这种死亡。研究论文的资深作者Anthony Letai博士曾发明一种叫做BH3检测的方法,可以检测细胞内占主导的信号是死亡前信号还是生存前信号。凋亡死亡信号占主导的肿瘤细胞更可能自杀,因此很容易通过治疗杀死;而生存前信号占主导的细胞就更耐受治疗。
在这项新研究中,研究人员检测了正常组织细胞的死亡倾向,结果发现成年人的大多数组织细胞,包括脑、心细胞几乎没有凋亡前信号,但是新生儿及儿童这些细胞的凋亡前信号很强烈,因此这些细胞在化疗或放疗时更容易死亡。
因为他们发现的凋亡分子涉及组织损伤,因此他们认为也许可以通过选择性抑制正常组织和细胞中的凋亡信号来降低化疗、放疗的毒性,同时维持肿瘤细胞对治疗的敏感性。“我们正在积极努力寻找可以达到这个目的的药物。”Sarosiek说道。
原始出处
Kristopher A. Sarosiek et al.Developmental Regulation of Mitochondrial Apoptosis by c-Myc Governs Age- and Tissue-Specific Sensitivity to Cancer Therapeutics.Cancer Cell.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#cancer cell#
27
#Cell#
26
#CEL#
27
#癌症儿童#
28
#放化疗#
37