Clin Gastroenterology H: 阻力训练可增加肝硬化患者的肌肉力量和肌肉大小
2020-05-01 MedSci原创 MedSci原创
肝硬化常因肌肉质量和强度下降而变得更棘手,这限制了患者进行日常活动的能力并影响生活质量。阻力训练可以增加老年人和慢性病患者的肌肉力量和质量。
背景与目标: 肝硬化常因肌肉质量和强度下降而变得更棘手,这限制了患者进行日常活动的能力并影响生活质量。阻力训练可以增加老年人和慢性病患者的肌肉力量和质量。因此,研究人员进行了一项随机对照试验,以研究抗阻力训练是否可以增加代偿性肝硬化患者的肌肉力量和质量。
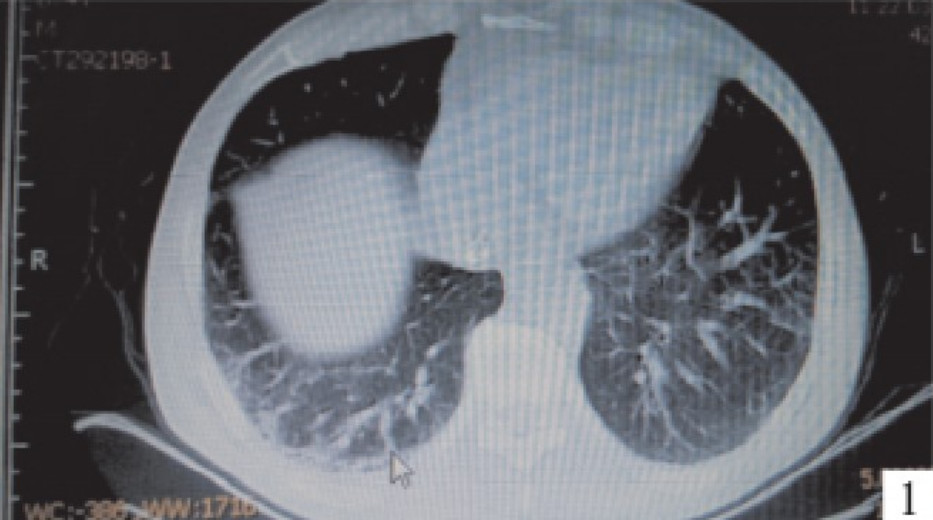
方法: 研究人员对2015年1月至2017年3月在丹麦的门诊就诊的39例肝硬化患者(Child-Pugh A级或B级儿童)进行了前瞻性研究。每天记录参与者的蛋白质摄入和活动水平。将参与者随机分配(1:1)到进行36次1小时的体育锻炼(有监督的进行性阻力训练1小时,每周3次,共12周)的组或对照组(每日活动水平无变化)。通过大腿的磁共振成像评估最大肌力,作为等速膝关节伸展时的峰值扭矩,测量肌肉大小。
结果: 运动组的肌肉力量增加了13%(从平均119 Nm增加到134 Nm),平均强度比对照组增加了11 Nm(P = 0.05)。运动组的股四头肌横截面积增加了10%(从平均58.5 cm 2增至64.6 cm 2),比对照组增加了4.4 cm 2(P <.01)。运动组的全身瘦体重和人体细胞质量显着增加,步行6分钟的路程和简短的36式问卷的精神成分摘要显着增加。
结论: 在一项对代偿性肝硬化患者进行的随机试验中,研究人员发现与不改变其日常活动常规的患者相比,有监督的进行性抵抗训练12周可增加肌肉力量和大小,并对总体表现指标产生有益的影响。
原始出处:
Luise Aamann. Et al. Resistance Training Increases Muscle Strength and Muscle Size in Patients With Liver Cirrhosis. Clin Gastroenterology H.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Gastroenterol#
42
#阻力训练#
43
#AST#
31
#GAS#
38
#Gastroenterology#
35
谢谢!最新的信息读起来就是收获大
52