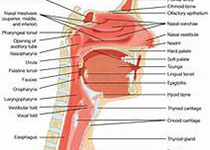
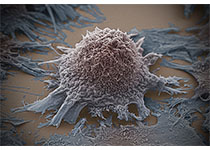
Oral Oncol:限量(化疗)放疗是口腔晚期鳞状细胞癌标准护理的另一有效选择
2017-12-16 lishiting MedSci原创
这篇研究的目的是为了比较标准治疗(手术组)和限量(化疗)放疗(CRT组)对晚期口腔癌(OCC)疗效的差异。尽管限量(化疗)放疗被认为对于疾病的控制要弱于手术疗法,但是关于此种方法疗效的数据却十分匮乏。
这篇研究的目的是为了比较标准治疗(手术组)和限量(化疗)放疗(CRT组)对晚期口腔癌(OCC)疗效的差异。尽管限量(化疗)放疗被认为对于疾病的控制要弱于手术疗法,但是关于此种方法疗效的数据却十分匮乏。研究通过表图评论的方法回顾分析了2000-2013年间的数据。旨在分析以下几个要点:局部控制(LRC)、无病生存(DFS)、疾病特异性生存(DSS)和总存活数(OS)。在CRT组(n=100)和手术组(n=109)之间,治疗前特征为平均分布,除了癌症的阶段和局部肿瘤直径(所有p≤.001)。在CRT组, 治疗5年后LRC比率为49%, DFS为22%, DSS为39%以及OS比率为22%。在手术组,治疗5年后的LRC比率为77%, DFS为45%, DSS为64%以及OS为45%。2组间LRC (p<.001), DFS和DSS (p=.001)以及OS (p=.002)的存活曲线具有明显差异。调整混杂因素和预后因素后,研究发现治疗组间的LRC存在显著性差异(调整HR=2.88, 95%CI 1.35-6.16, p=.006)。在治疗100天内,CRT组中有5名患者(5%)死于治疗
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#细胞癌#
45
#Oral#
33
学习了谢谢作者分享!
64
#Oncol#
45
学习了新知识
54
学习并分享!!
54