Ann Oncol:内分泌联合或不联合abemaciclib(阿贝西利)辅助治疗HR+/HER2-早期高危乳腺癌患者的疗效
2021-12-02 yd2015 MedSci原创
研究表明,abemaciclib + ET辅助治疗HR+/HER2-早期高危乳腺癌患者可改善IDFS,不管KI-67高低如何。
monarchE (NCT03155997)是一项全球、开放标签、随机III期临床研究。主要评估在HR+/HER2-早期高危乳腺癌患者中,内分泌治疗联合或不联合abemaciclib(阿贝西利)辅助治疗的疗效。研究证明abemaciclib(阿贝西利)的加入可提高无浸润生存期(IDFS)和远处无复发生存期(DRFS)。近期,Annals of Oncology杂志更新了该研究的研究成果。
该研究将5637 例患者随机(1:1)分配至ET辅助治疗(≥5年)联合或不联合abemaciclib(2年)。队列1纳入的患者为腋窝淋巴结(ALN)阳性≥4,或1-3个阳性ALN,以及G3或肿瘤≥5cm。队列2纳入患者为1-3个阳性ALN,以及高KI-67(≥20%)。主要研究终点为ITT人群(队列1和2)的IDFS,次要终点为高Ki-67患者的IDFS,DRFS,OS和安全性。
共有5637例患者随机接受abemaciclib + ET (n=2808)或单独ET (n=2829)治疗。队列1中有5120例患者。全队列人群和队列1人群中分别有44.3%和39.1%的患者为高KI-67患者。队列1人群中有37.4%患者为低KI-67患者。
在中期分析达到统计学意义后,ITT人群中中位随访19个月时(PO),abemaciclib + ET继续在IDFS中获益 (HR=0.71, 95%CI 0.58-0.87;p<0.001)。2年IDFS率也有3.0%的绝对改善(abemaciclib + ET: 92.3% vs单独ET: 89.3%)。同样,abemaciclib + ET也可继续改善患者 DRFS(HR=0.69, 95%CI 0.55-0.86;p<0.001),对应2年DRFS率分别为93.8%和90.8%。
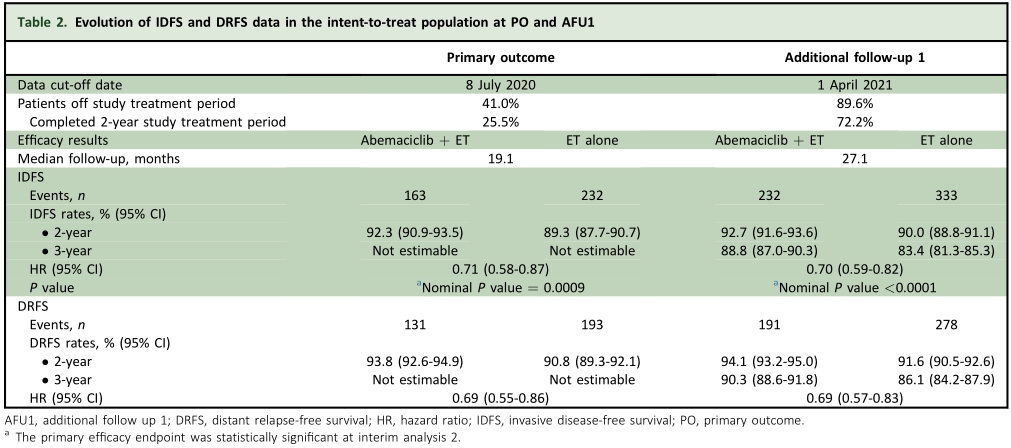
疗效汇总
延长随访时间至中位27个月时(AFU1),abemaciclib +ET仍然维持对于IDFS(HR=0.70, 95% CI 0.59-0.82; nominal P < 0.0001) 和DRFS (HR=0.69, 95% CI 0.57-0.83; nominal P < 0.0001)的获益。3年IDFS率分别为88.8%和83.4%;而3年DRFS率分别为90.3%和86.1%。
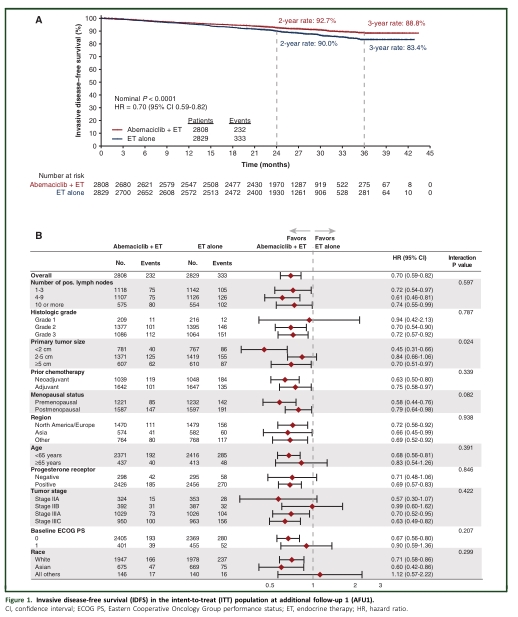
ITT AFU-1分析
ITT伴有高KI-67患者中,中位随访19个月时(PO),abemaciclib +ET治疗降低31% IDFS风险 (HR=0.69, 95% CI 0.52-0.92,p=0.0111)。2年IDFS率分别为91.6%和87.1%;而2年DRFS率分别为90.3%和86.1%。随访时间至中位27个月时(AFU1),abemaciclib +ET治疗降低34% IDFS风险(HR=0.66, 95% CI 0.52-0.84; nominal P=0.0006),降低36% DRFS风险(HR=0.64, 95% CI 0.49-0.83; nominal P =0.0006)。
队列1伴有高KI-67患者中,中位随访19个月时(PO),abemaciclib +ET治疗降低36% IDFS风险 (HR=0.64, 95% CI 0.48-0.87; two-sided P=0.0042)。2年IDFS率分别为91.3%和86.1%;而低KI-67患者中,IDFS有有所改善(HR=0.69, 95% CI 0.46-1.02;p=0.059)。2年IDFS率分别为94.8%和92.0%。
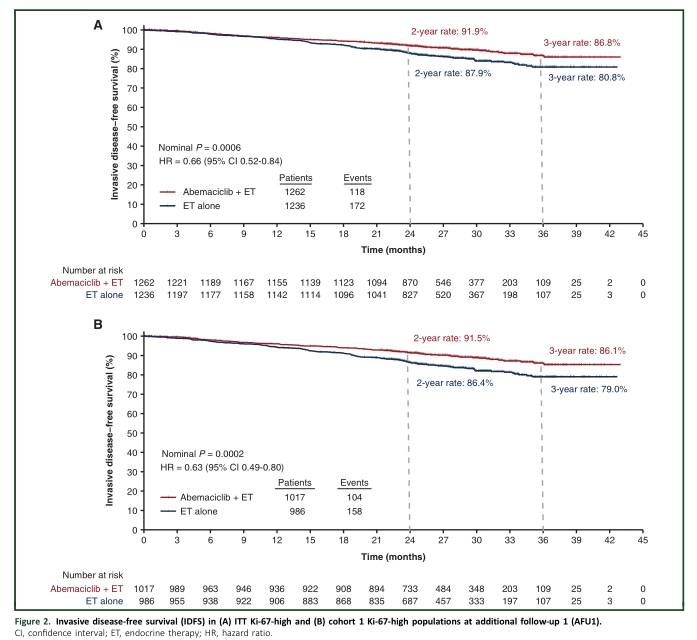
高KI-67患者预后分析
随访时间至中位27个月时(AFU1),队列1伴有高KI-67患者中abemaciclib +ET治疗降低37% IDFS风险(HR =0.63, 95% CI 0.49-0.80; nominal P=0.0002),降低40% DRFS风险(HR= 0.60, 95% CI 0.46-0.79; nominal P=0.0002)。低KI-67患者中也可改善IDFS(HR=0.70, 95% CI 0.51-0.98; nominal P=0.036)。
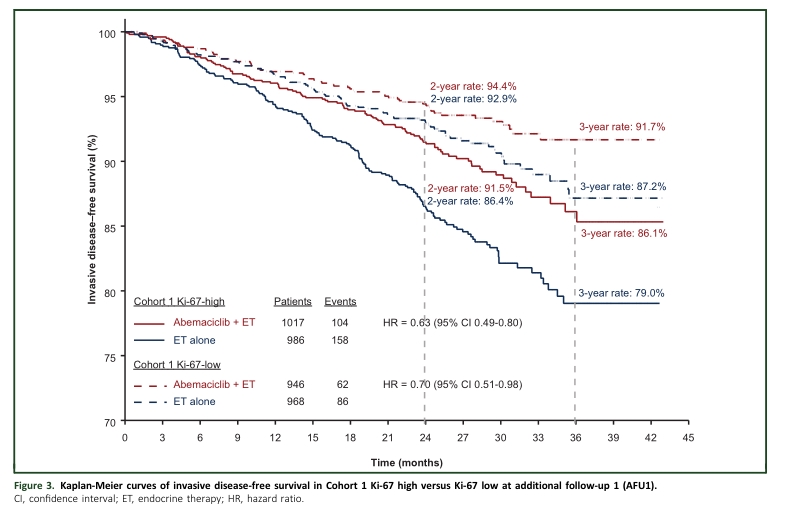
高低KI-67患者对比
在AFU1,治疗中位持续时间为24个月。abemaciclib + ET与单独ET相比,3级AEs和严重AEs的发生率更高(分别为50% vs 16%和15%vs9%)。
综上,研究表明,abemaciclib + ET辅助治疗HR+/HER2-早期高危乳腺癌患者可改善IDFS,不管KI-67高低如何。
原始出处:
Harbeck N, Rastogi P, Martin M, et al; monarchE Committee Members. Adjuvant abemaciclib combined with endocrine therapy for high-risk early breast cancer: updated efficacy and Ki-67 analysis from the monarchE study. Ann Oncol. 2021 Dec;32(12):1571-1581. doi: 10.1016/j.annonc.2021.09.015. Epub 2021 Oct 14. PMID: 34656740.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#分泌#
36
#Oncol#
31
#MAC#
38
#HER2-#
25
#EMA#
24
#乳腺癌患者#
31
学习了
50