Clin Cancer Res:曲妥珠单抗联合内分泌或化疗作为HR+HER2+转移性乳腺癌的一线治疗的疗效对比
2021-11-23 Nebula MedSci原创
曲妥珠单抗联合内分泌治疗作为激素受体阳性、HER2阳性的转移性乳腺癌的一线方案的效果不劣于曲妥珠单抗联合化疗
约10%的转移性乳腺癌(MBC)患者的激素受体(HR)和人表皮生长因子受体2(HER2)都是阳性。抗HER2疗法联合化疗作为HER2+转移性乳腺癌的一线治疗已展现出了生存效益。
目前还没有研究证据表明,在激素受体阳性和人表皮生长因子受体2阳性转移性乳腺癌的一线治疗中,内分泌治疗或化疗哪个是联合抗HER2治疗更好的伴侣策略。
本研究旨在对比曲妥珠单抗联合内分泌治疗 vs 曲妥珠单抗联合化疗作为HR阳性和HER2阳性转移性乳腺癌的一线治疗策略的疗效和安全性。
这是一项在中国的9家医院开展的开放标签、非劣效的、随机对照的3期临床试验。招募了HR阳性和HER2阳性转移性乳腺癌患者,随机分成两组,接受曲妥珠单抗联合内分泌治疗(ET 组)或曲妥珠单抗联合化疗(CT 组),并根据既往辅助内分泌疗法和疾病状态(复发 vs 新发转移)进行分层。主要终点是无进展生存期(PFS),风险比的非疗效性上限是1.35。
无进展生存期
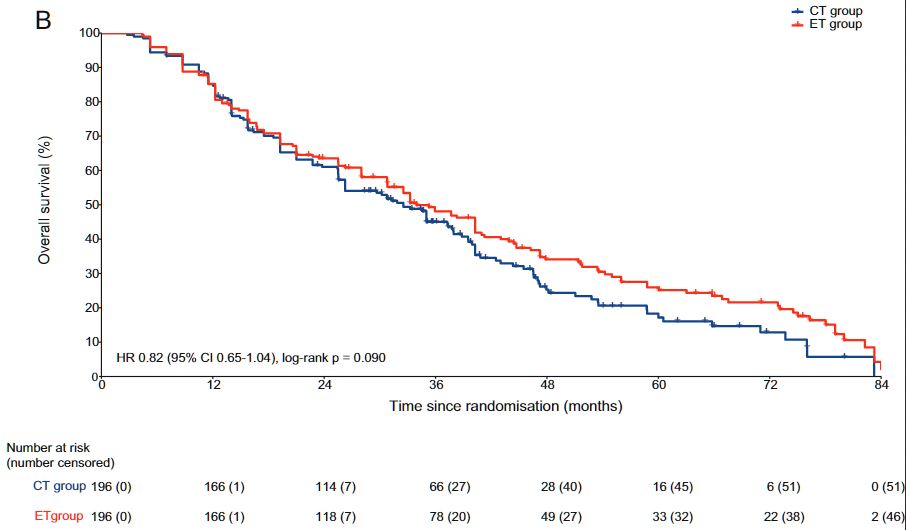
共招募了392位患者,ET 组 196位,CT 组 196位。中位随访了30.2个月(IQR 15.0-44.7)后,ET 组和CT 组的中位PFS分别是19.2个月(95% CI 16.7-21.7)和14.8个月(12.8-16.8; 风险比 0.88, 95% CI 0.71-1.09;p<0.0001)。ET 组和 CT 组的中位总生存期分别是33.9个月和32.5个月(HR 0.82,95% CI 0.65-1.04;p=0.094)。与ET 组相比,CT 组的毒性反应发生率明显更高。
总生存期
综上,曲妥珠单抗联合内分泌治疗作为激素受体阳性、HER2阳性的转移性乳腺癌的一线方案的效果不劣于曲妥珠单抗联合化疗。
原始出处:
Xin Hua, Xi-wen Bi, Jian-Li Zhao, et al. Trastuzumab Plus Endocrine Therapy or Chemotherapy as First-line Treatment for Patients with Metastatic Breast Cancer with Hormone Receptor-positive and HER2-positive (SYSUCC-002). Clin Cancer Res November 22 2021 DOI:10.1158/1078-0432.CCR-21-3435
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#分泌#
42
#曲妥珠#
54
学习了
63
#转移性#
41
坚持学习
69