NEJM:食管癌的混合微创食管切除术疗效分析
2019-01-10 xing.T MedSci原创
由此可见,该研究发现混合微创食管切除术导致术中和术后主要并发症,特别是肺部并发症的发生率低于开放性食管切除术,而不会影响3年内的整体和无病生存率。
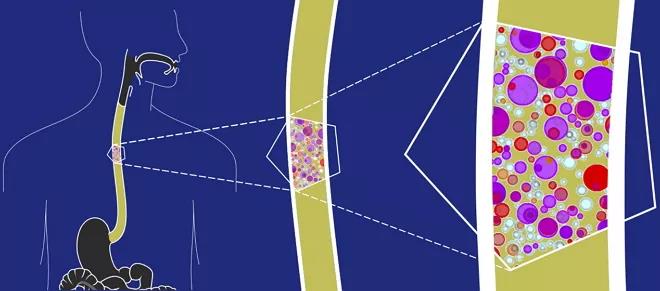
术后并发症,尤其是肺部并发症,影响了超过一半的接受开放式食管切除术的食管癌患者。混合微创食管切除术是否比开放式食管切除术得到更低的发病率尚不清楚。
近日,顶级医学期刊NEJM上发表了一篇研究文章,研究人员进行了一项多中心、开放标签、随机对照试验,该试验涉及18至75岁患有可切除的食管中下三分之一的癌症患者。患者被随机分配接受经胸开放式食管切除术(开放手术)或混合微创食管切除术(混合手术)。通过外科医生的资格认证,技术的标准化和性能监测来实施手术质量保证。混合手术包括腹部双胸腹部手术(也称为Ivor-Lewis手术)、腹腔镜胃动员和开胸右侧胸廓切开术。该研究的主要终点是在30天内根据Clavien-Dindo分类(需要干预的主要并发症指征)的II级或更高级别的术中或术后并发症。根据意向治疗原则进行分析。
从2009年10月到2012年4月,研究人员将103名患者随机分配到混合手术组,104名患者随机分配到开放手术组。110名患者共记录了312次严重不良事件。混合手术组共有37例患者(36%)出现术中或术后并发症,而开放手术组为67例(64%)(比值比为0.31; 95%置信区间[CI]为0.18至0.55; P<0.001)。混合手术组中102名患者中的18名(18%)患者出现严重的肺部并发症,而开放手术组中的103名患者中有31名(30%)。在3年时,混合手术组的总生存率为67%(95%CI为57-75),而开放手术组为55%(95%CI为45-64); 无病生存率分别为57%(95%CI为47-66)和48%(95%CI为38-57)。
由此可见,该研究发现混合微创食管切除术导致术中和术后主要并发症,特别是肺部并发症的发生率低于开放性食管切除术,而不会影响3年内的整体和无病生存率。
原始出处:
Christophe Mariette,et al.Hybrid Minimally Invasive Esophagectomy for Esophageal Cancer.NEJM.2019.https://www.nejm.org/doi/full/10.1056/NEJMoa1805101
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#切除术#
30
#食管切除术#
39
#疗效分析#
20
#微创#
24
#食管#
24
谢谢梅斯提供这么好的信息,学到很多
37