Lancet Oncol:纳武单抗用于dMMR/MSI-H转移性结直肠癌显示出了令人鼓舞的疗效
2017-07-28 王东亮 肿瘤资讯
本研究为纳武单抗治疗转移性dMMR/MSI-H结直肠癌患者的Ⅱ期临床试验,纳武单抗的疗效优于既往传统治疗,且疗效及疾病控制维持时间持久,不受基因状态及亚组分组因素影响,为这部分患者开启了免疫治疗的全新篇章。 概述 结直肠癌是全球高发肿瘤之一,不能接受手术的转移性结直肠癌患者只能接受氟尿嘧啶药物为基础的化疗方案,也可以选择是否联合抗血管生成或抗EGFR治疗,这部分患者的五年生存率仅为13.5
本研究为纳武单抗治疗转移性dMMR/MSI-H结直肠癌患者的Ⅱ期临床试验,纳武单抗的疗效优于既往传统治疗,且疗效及疾病控制维持时间持久,不受基因状态及亚组分组因素影响,为这部分患者开启了免疫治疗的全新篇章。
概述
结直肠癌是全球高发肿瘤之一,不能接受手术的转移性结直肠癌患者只能接受氟尿嘧啶药物为基础的化疗方案,也可以选择是否联合抗血管生成或抗EGFR治疗,这部分患者的五年生存率仅为13.5%。近年间有研究表明DNA错配修复功能缺失(DNA mismatch repair defcient,dMMR)或微卫星不稳定(Microsatellite instability-high, MSI-H)转移性结直肠癌患者接受传统治疗效果不佳,生存期短于DNA错配修复功能正常(profcient MMR, pMMR)群体。dMMR/MSI-H结直肠癌患者的特点为肿瘤的突变负荷、新生抗原较高,肿瘤中浸润的淋巴细胞数量较高。一项汇总研究发现,在4项Ⅲ期研究中,dMMR转移性结直肠癌的一线治疗效果显着差于pMMR患者(OS 13.6 vs 16.8个月,HR=1.35,95%CI 1.13-1.61,p=0.001)。尽管如此,传统化疗及靶向治疗针对dMMR患者并无特定方案,而由于其错配功能缺失,肿瘤内在突变数目较多,产生了大量的新生抗原,导致大量淋巴细胞浸润到了肿瘤中的微环境之中,所以,以PD-1为代表的免疫拮抗点抑制剂可能会对这部分患者有一定的帮助。在一项Ⅰ期研究中,观察纳武单抗用于治疗难治性dMMR实体瘤,在39名患者中没有14名患者为转移性结直肠癌,并且有一名患者疾病完全缓解持续长达3年。在既往研究的基础上,研究者设计了CheckMate142研究用于观察纳武单抗单药或联合伊匹单抗治疗MSI-H及非MSI-H的转移性结直肠癌患者的疗效及安全性。本文仅介绍纳武单抗治疗MSI-H转移性结直肠癌患者内容。
方法及过程
本研究于8个国家31个中心招募了MSI-H的转移性结直肠癌患者,入组标准为18岁以上,体力评分0-1分,组织学确定的dMMR或MSI-H肠癌,且疾病处于转移或复发阶段,患者需至少接受过一次含氟尿嘧啶类药物联合奥沙利铂或伊立替康的治疗后出现疾病进展或不耐受。患者每两周接受一次3mg/kg剂量的纳武单抗单药治疗直至疾病进展,死亡、不可接受的毒副作用,或主动退出及研究终止。纳武单抗的剂量不允许减量,但可以依据药物相关不良反应而停药6周内的再次应用。当疾病出现首次进展且肿瘤负荷增加在10%以内时,在患者可以耐受的情况下,研究者可以依据判断而决定患者可以继续应用纳武单抗。肿瘤的MMR/MSI状态免疫组化或PCR方法来评估认定,MSI状态的认定由中心实验室应用PCR方法(修改的Bethesda方法,其中包括TGFβR-2)检测新鲜活检组织得出微卫星稳定的标志物阳性数量。肿瘤PD-L1的检测应用Dako28-8免疫组化试剂盒检测。林奇综合征由研究者依据患者既往史来认定,本研究不强制进行遗传检测。本研究的主要研究终点为研究者依据RECIST1.1标准所评估的客观缓解率,其中包括最佳缓解率,疗效维持时间及完全缓解率。次要研究终点为独立中心评估的客观缓解率,探索性研究终点为纳武单抗的安全性及耐受性,研究者及独立中心评估的无进展生存期,总生存及与PD-L1的表达、纳武单抗疗效及生活质量改变的关联。
结果
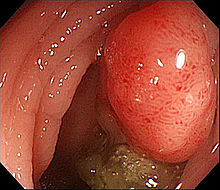
自2014年3月至2016年3月,74名dMMR/MSI-H转移性结直肠癌入组到本研究,大多数患者年纪均小于65岁,既往接受过三线甚至多线系统治疗,有4名患者既往仅接受过辅助治疗而在转移阶段未接受过治疗,29(39%)名患者为BRAF、KRAS野生型,12名(16%)患者为BRAF突变。研究数据截止在2017年1月时,仍有36名(49%)患者仍在接受治疗。23名患者获得了客观缓解,51名患者在接受纳武单抗治疗12周时疾病得到了控制(图1)。患者的疾病对纳武单抗出现响应的中位时间为2.8个月,疾病缓解及稳定的时间都很持久,仅有3名患者在初始治疗疾病缓解后出现了疾病进展,在研究数据截止时,中位疾病缓解持续时间尚未达到,并且所有疾病得到响应的患者均未发生死亡,有8名患者的疗效维持时间长于1年。当出现了36个疾病进展事件后,本研究的中位无进展生存期为14.3个月,12月无进展生存率为50%,12月总生存率为73%,中位生存期未达到(图2)。有99%的患者都报告了各种因素导致的不良反应,39%的患者不良反应为1-2级,41%的患者为3级,14%的患者报告的不良反应为4级,5%的患者死于与治疗不相关的原因(一例突然死亡,一例心功能障碍,两例疾病进展)。70%的患者报告了药物相关的副作用,20%的患者不良反应为3或4级,常见的不良反应为脂肪酶、淀粉酶升高。有5名患者由于药物相关的副作用而导致治疗终止,主要原因为ALT升高,结肠炎,十二指肠溃疡,急性肾损伤及胃炎。
本项开放式、多中心、Ⅱ期临床研究,纳武单抗用于治疗dMMR/MSI-H转移性结直肠癌患者显示出了令人鼓舞的疗效,并且其疗效横跨各项亚组,患者是否为林奇综合征,BRAF、KRAS基因突变与否,甚至包括PD-L1≥1%或<1%的患者群体,提示PD-L1的表达并不是纳武单抗治疗这部分患者的疗效预测因素。并且,本研究观察到BRAF突变的患者群体中,客观有效率可达到25%,要高于既往研究报道的化疗(小于10%)、靶向治疗(BRAF、EGFR或MEK抑制剂,10-16%)。所以,本研究较为意外的发现纳武单抗针对肠癌中BRAF突变预后较差的群体有较好的治疗效果。并且,本研究的生存曲线、无进展生存期曲线都出现了平台期,截止数据发表时,中位生存期尚未达到。本研究中,纳武单抗可以改善患者的生活质量并可以很好的为患者耐受,常见的严重不良反应为脂肪酶、淀粉酶升高,与既往实体瘤研究中一致。由于结直肠癌发病年龄普遍较大,但dMMR/MSI-H患者群体年纪较轻,本研究为这部分患者提供了很好的数据及证据支持。总而言之,本研究对dMMR/MSI-H患者,这一既往疗效不佳、预后较差的群体提供了崭新的治疗方式。
专业点评:自从帕姆单抗治疗错配修复功能缺失肿瘤2年前ASCO与新英格兰医学杂志上惊艳亮相之后,PD-1单抗就与这一类肿瘤形成了“一堆捧哏与逗哏的黄金搭档”,没事就拎出来虐一虐,相关研究结果均高歌猛进,直至今年5月份,美国FDA宣布:加速批准帕姆单抗用于dMMR/MSI-H成人及儿童晚期或转移性实体肿瘤患者——这是FDA首次不以肿瘤来源部位为限定,仅依靠肿瘤基因状态而批准的药物。帕姆单抗的相关研究也于今年6月刊登于《科学》杂志,结果依然是十分的傲娇:在总计86名dMMR进展期肿瘤患者中,帕姆单抗取得了高达54%的客观缓解率,并且有21%的完全缓解率,疾病控制率可达77%,在这86名患者中有40名肠癌患者,仅完全缓解率低于总体水平,但其他数据均好于或等于总体患者水平。而本次报道的CheckMate-142研究数据,则还是要逊色一些。要是回头看,为什么KEYNOTE-024研究成功了,CheckMate-026研究结果未能达到研究终点?可能我们都会说两个申办方分别以不同的肿瘤PD-L1的表达情况来纳入了不同的患者,但前段时间我们仔细分析了CheckMate-026研究中PD-L1大于50%的患者群体中,纳武单抗依然未能优于化疗,而我们的的确确不能认定这两个药物的疗效会存在本质上的区别,所以,纳武单抗这种情况不是第一次出现了。不过,好在,dMMR/MSI-H患者的化疗效果实在是太差了。不过,纳武单抗的研究数据的确没能从数值上达到既往帕姆单抗的研究结果,但我们需要注意的是,纳武单抗的背后总是闪现着“魔铃”一般的影子——伊匹单抗,要知道每当纳武单抗(星矢)遇到困难时,无论是打开还是爆炸他的小宇宙,他们姐弟俩个一起战斗时,战斗力总是处于爆表状态,CheckMate-026研究纳武单抗单药失败了也不怕,后续还有双药方案。CheckMate-142研究数据不理想?也不怕,这次只是先把弟弟的结果提前放送出来,告诉大家单药肯定比化疗强(星矢已经不是一般的青铜圣斗士)就是了,研究的整体数据还有待于进一步的发表,将来一切皆有可能。毕竟主要竞争对手帕姆单抗那边也并不是一帆风顺的,KEYNOTE-040研究,帕姆单抗对比标准化疗治疗进展期头颈部鳞癌就未能达到OS研究终点。所以,别急,他们终归都会赢的,只要挑选对了对手(不要太相信PD-L1),没有拿不下的适应症。
原始出处:
Michael J Overman, Ray McDermott, et al. Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142) an open-label, multicentre, phase 2 study. The Lancet Oncology Published: 19 July 2017
dx.doi.org/10.1016/S1470-2045(17)30422-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncol#
40
#dMMR/MSI-H#
41
#Lancet#
32
#转移性#
42
#结直肠#
47
#MMR#
53
#MSI#
38
学习一下谢谢分享
66
学习了受益匪浅
82
学习谢谢分享
65