JOT:肱骨远端骨折内固定钢板的生物力学研究
2014-05-16 佚名 丁香园
肱骨远端骨折,约占全身骨折的2%,是一种具有挑战性的复杂创伤。通常需行切开复位内固定,以期获得良好的功能恢复。但手术治疗后仍有20%-25%的患者疗效欠佳。潜在的手术并发症包括:局部粘连、关节活动范围减小、神经功能丧失、伸直受限、创伤后退行性关节炎、各种感染、缺血性坏死及内固定失效等。内固定失效往往是由内固定技术的缺陷造成的。 如何避免内固定失效这一并发症,尤其在骨质条件较差的患者群中,将指
肱骨远端骨折,约占全身骨折的2%,是一种具有挑战性的复杂创伤。通常需行切开复位内固定,以期获得良好的功能恢复。但手术治疗后仍有20%-25%的患者疗效欠佳。潜在的手术并发症包括:局部粘连、关节活动范围减小、神经功能丧失、伸直受限、创伤后退行性关节炎、各种感染、缺血性坏死及内固定失效等。内固定失效往往是由内固定技术的缺陷造成的。
如何避免内固定失效这一并发症,尤其在骨质条件较差的患者群中,将指导肱骨远端骨折内固定金标准的制定。尽管之前有研究涉及常规加压钢板与锁定钢板在平行位置与垂直位置的生物力学,但尚无一项独立研究测试所有组合的可能性。美国学者Caravaggi等进行了一项新的生物力学研究,来探讨相关问题。
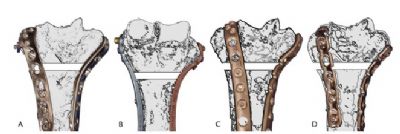
该项研究将取自14具尸体的28根肱骨随机分为4组。测试前去除所有软组织并冷冻待用。所有肱骨均经放射学评估,无明显骨质破坏等问题,人为造成距离关节面4cm的宽为5mm的骨折线。分组如下:IMP1:Synthes的锁定钢板,置于内侧及后外侧;IMP2:Acumed的平行锁定钢板;IMP3:Smith & Nephew的锁定钢板,垂直放置;IMP4,Synthes3.5mm重建钢板垂直放置(后外侧及内侧)。
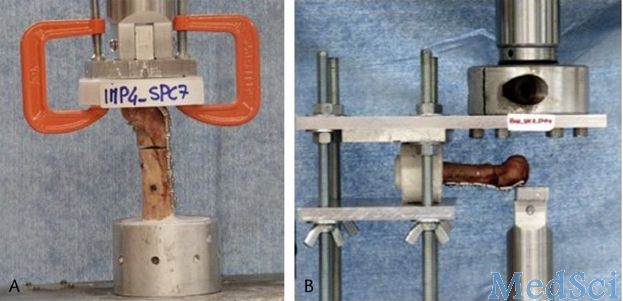
IMP1,2,3组使用锁定方式固定,IMP4组采用非锁定固定。远折端的所有锁定螺钉孔均置入锁定螺钉,并确定所有螺钉足够长。如图1所示:
测试结果发现:承载方面:IMP2组在轴向加压后表现出最大的刚度,而IMP1组刚度最差。 IMP1,2,3组在承受前后屈曲载荷时表现出类似的刚度,且三组均显著优于IMP4组。疲劳试验方面:IMP1,2,3组在承受5000个周期之后,永久形变均小于5mm。IMP4组的永久变形平均为1.44mm,与IMP1,2,3组相比存在显著性差异。在平均极限强度方面,IMP2组表现出最强的结构强度。
塑性变形和植入物松动,或者两者均存在,是所有组别中的3种主要失效模式。IMP2组中只有1例发生骨-植入物界面的突然失效。由该项研究结果不难看出,平行锁定钢板组表现出轴向的最大刚度和最高的极限强度。平行钢板内固定与垂直钢板比较,所有锁定组的测试中在矢状面强度和疲劳试验中无明显差别。与非锁定结构相比,锁定结构在所有的测试中均优于非锁定组。
在极限强度测试中,所有组都会存在变形和松动。虽然该研究表明,平行锁定钢板比垂直锁定钢板和3.5mm重建钢板能提供更高强度的内固定,但平行置板需要的手术操作技术更具挑战性。具体的置板方式,有时还要取决于骨折的类型。外侧柱完全显露,往往需要过多的软组织剥离。某些情况下,后侧入路置入后外侧钢板来固定外侧柱,在手术技术上更容易操作。
因此,虽然平行置板在实验室研究中表现优良,但临床应用中并非总是最佳选择。虽然先后有人进行了类似研究,但哪种内固定结构方式最适合于肱骨远端骨折的治疗,尚未达成广泛共识。进一步的研究探索仍是必要的。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#骨折内#
40
#生物力学研究#
28
#肱骨远端#
41
#肱骨#
24
#内固定#
35