J Thorac Oncol:2017年胸部恶性肿瘤进展
2018-01-19 慧语 转化医学网
2017年,可谓是非小细胞肺癌(NSCLC)治疗史上的大年。对基于驱动基因的NSCLC(EGFR突变和ALK重排),与第一代酪氨酸激酶抑制剂(TKI)相比,新一代TKI(如osimertinib或alectinib)已经显示出更好的缓解率和无进展存活。免疫检查点抑制剂(ICIs)对未经治疗的PDL1表达≥50%的患者显示出良好的治疗缓解和总生存(OS)。此外,抗PD-1 / PD-L1抑制剂与化疗
2017年,可谓是非小细胞肺癌(NSCLC)治疗史上的大年。对基于驱动基因的NSCLC(EGFR突变和ALK重排),与第一代酪氨酸激酶抑制剂(TKI)相比,新一代TKI(如osimertinib或alectinib)已经显示出更好的缓解率和无进展存活。免疫检查点抑制剂(ICIs)对未经治疗的PDL1表达≥50%的患者显示出良好的治疗缓解和总生存(OS)。此外,抗PD-1 / PD-L1抑制剂与化疗或抗CTLA4抑制剂的新组合也展现了令人信服的初步结果。虽然NSCLC的治疗取得了突破性的进展,但NSCLC靶向治疗中用药顺序如何确定?免疫疗法中如何预测患者的敏感性、生物标志物如何鉴定以及如何针对患者制定最佳治疗组合?这些问题都给肺癌治疗带来了非常大的挑战,肺癌的治疗依旧任重而道远。《Journal of Thoracic Oncology》杂志梳理了2017年NSCLC治疗的重要临床研究。
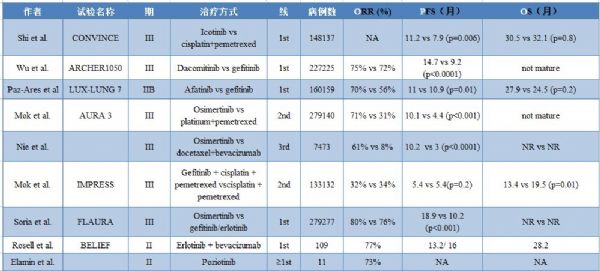
首先不得不提的是对于EGFR突变NSCLC腺癌治疗手段的研究,在过去一年可谓百花齐放、百家争鸣,出现了多个具有竞争力的新药。主要临床试验和结果参见下表(表1)。
表1 2017年发表的EGFR突变的非小细胞肺癌临床研究
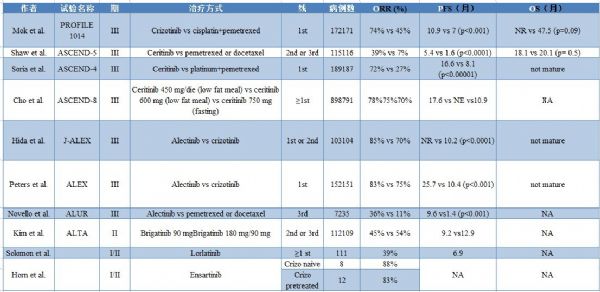
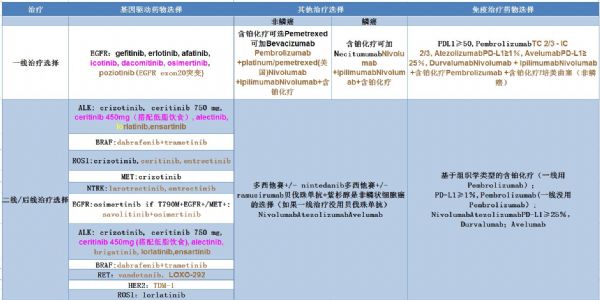
2017年,对于ALK重排的NSCLC患者,治疗方面同样取得了重大的进展,经过适当治疗,OS可延长至7.5年。但并非所有的ALK融合都有类似的效果,具有Variant 3a/b的患者就对ALK TKIs不敏感,原因可能是蛋白质稳定性较高。次要的ALK抗性突变可以通过无细胞DNA监测更好的了解抗性机制。 表2总结了2017年期间ALK重排的NSCLC患者的主要临床试验,表3总结了2017年发表的无EGFR突变、无ALK重排的NSCLC患者的临床研究。同时,表4总结了当前非小细胞肺癌的治疗标准和顺序,并强调了新的治疗选择。
表2 2017年发表的ALK重排的非小细胞肺癌临床研究
表3 2017年发表的无EGFR突变、无ALK重排的非小细胞肺癌临床研究
表4 非小细胞肺癌目前的标准疗法和新的选择
注:橙色基于I-II期研究结果;紫色基于III期研究结果。
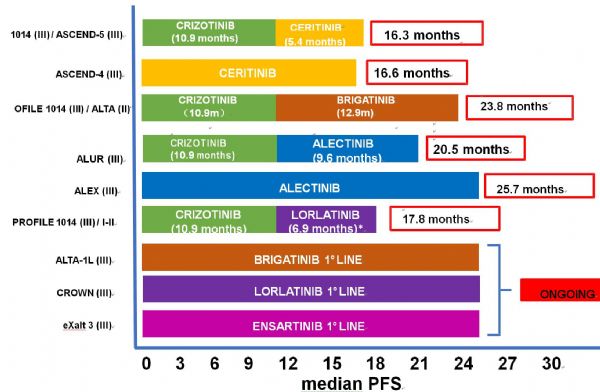
考虑到第一代和第二代EGFR TKI药物在NSCLC患者中的优异疗效,加上目前还缺乏成熟的OS数据,所以关于各代TKI药物的最佳治疗顺序似乎还不能得出确定性结论,图1列出各研究中TKI治疗顺序的组合和相应的PFS,仅供参考。此外,尽管取得了很多令人鼓舞的结果,但关于最佳治疗策略和组合的许多问题仍未得到解答,如图2所示。
图1 各代EGFR TKIs治疗顺序对于EGFR突变的NSCLC的治疗策略和相应PFS
图2 各项研究中的治疗策略和组合
总 结
在2017年期间,晚期非小细胞肺癌涌现出了多项研究,免疫治疗证实在二线治疗和PD-L1表达≥50%患者的一线治疗的长期存活益处。在一线治疗中,抗PD-1 / PD-L1药物联合化疗或抗CTLA-4治疗初步显示了良好的结果。在EGFR或ALK阳性NSCLC患者中,预测性生物标志物(特别是PD-L1)可用于鉴定潜在的受益者。此外,初步数据表明免疫治疗可以获得长期益处,但疗效和毒副作用很可能呈相关性。在二线或后线治疗中,PD-L1并不是阿特珠单抗(atezolizumab)的可靠生物标志物,其他的预测生物标志物(如TMB)或许更好。此外,免疫治疗期间的肿瘤加速生长的患者,首次被认为是预后更差的NSCLC亚组。
对于突变癌基因驱动的非小细胞肺癌,与第一代药物相比,新一代EGFR TKI药物(osimertinib)和ALK药物(alectinib)显示出良好的疗效和PFS。 新的强效药物(lorlatinib,entrectinib和larotrectinib)在ROS-1或NTRK重排的NSCLC中的治疗表现令人鼓舞。 最后,RET重排和BRAF、MET外显子14及HER2突变成为了新的可靶向致癌的驱动因子,对不同的TKI单药或组合用药(如dabrafenib与trametinib联合用于BRAF突变的NSCLC患者)有良好的反应。
另一方面,2017年,SCLC,MPM和胸腺恶性肿瘤的治疗没有大的变化。初步数据表明免疫治疗、抗DDL3疗法(RovaT)和新的化学药物(lurbinectedin)可能对于SCLC有效。 此外,免疫治疗在MPM或胸腺恶性肿瘤中显示可喜的疗效,未来将有望为医生和患者提供新的治疗选择。
原始出处:
Roberto Ferrara, et al.,Progress in the Management of Advanced Thoracic Malignancies in 2017.J Thorac Oncol.January 10, 2018.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#肿瘤进展#
36
#THORAC#
29
#Oncol#
33
#胸部恶性肿瘤#
38
学习一下知识
57
学习谢谢分享
49
认真学习天天向上
57
谢谢分享
62
学习学习
64
学习了谢谢作者分享!
17