Cancer Cell:特异性抑制自噬治疗肾细胞癌
2012-04-20 Beyond 生物谷
美国辛辛那提大学(UC)研究人员完成的一项新研究表明,肾癌细胞的生长依赖于细胞吞噬,细胞吞噬是一个可以从内部提供给肿瘤细胞营养物质的复杂过程。研究人员说自噬在某些情况下可保护接受化疗的肿瘤细胞,使肿瘤细胞能够在休眠状态、转移状态过程中存活很长一段时间。 在这项新公布的研究数据中,研究人员von Hippel-Lindau肿瘤抑制基因或VHL中确定了两种截然不同的自噬调控通路。这种特定的肿瘤抑制基
美国辛辛那提大学(UC)研究人员完成的一项新研究表明,肾癌细胞的生长依赖于细胞吞噬,细胞吞噬是一个可以从内部提供给肿瘤细胞营养物质的复杂过程。研究人员说自噬在某些情况下可保护接受化疗的肿瘤细胞,使肿瘤细胞能够在休眠状态、转移状态过程中存活很长一段时间。
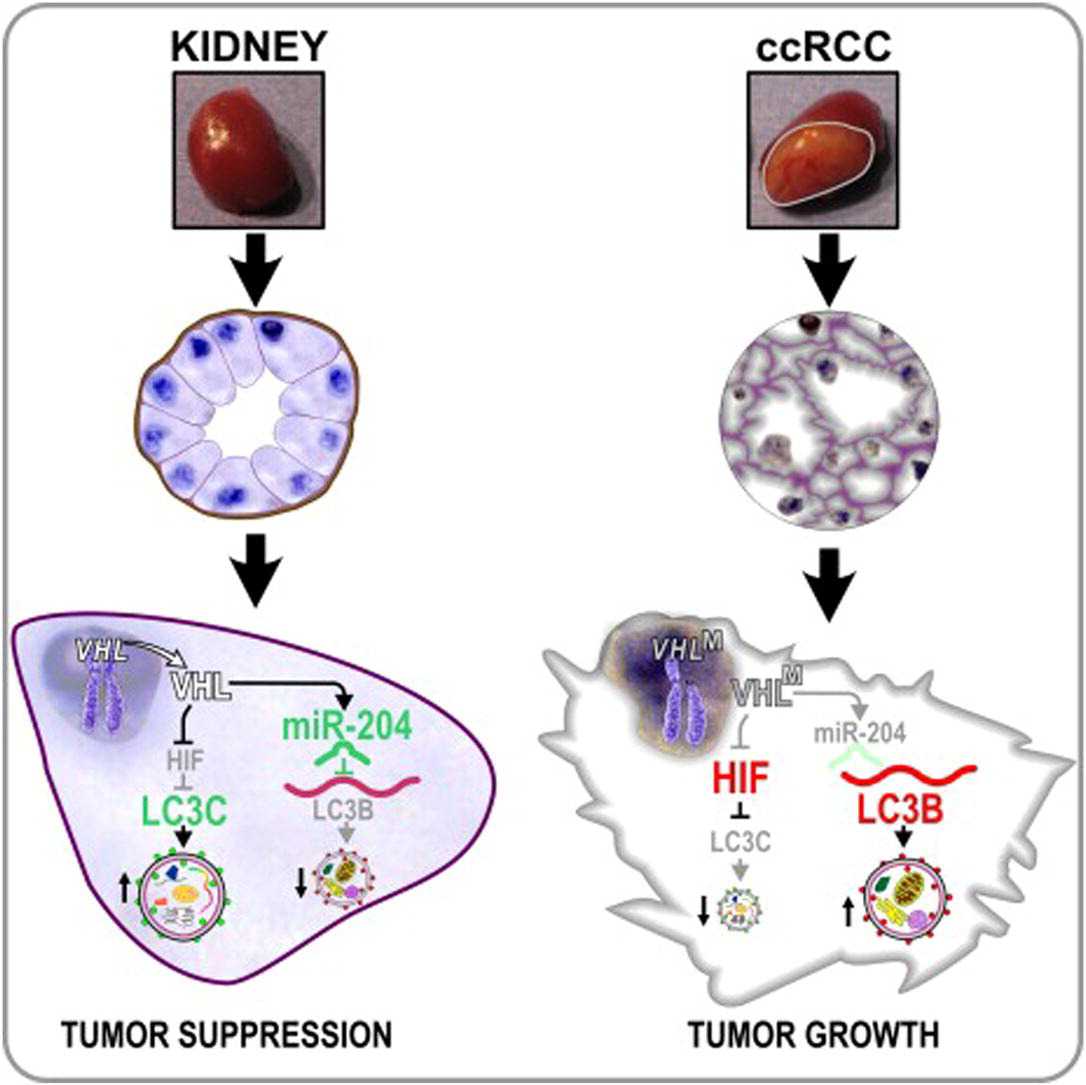
在这项新公布的研究数据中,研究人员von Hippel-Lindau肿瘤抑制基因或VHL中确定了两种截然不同的自噬调控通路。这种特定的肿瘤抑制基因在大多数肾细胞癌中都是缺失的。

加州大学研究人员将这些研究结果发表在4月16日的Cancer Cell杂志上。
Maria Czyzyk-Krzeska博士说:这些发现可以指导研究人员认识具体的自噬过程,对肾细胞癌特别是转移性肾细胞癌采取更有效的治疗方法。
Czyzyk Krzeska解释:我们的研究工作表明肿瘤细胞有不同的自噬过程,促进或是抑制肿瘤。肿瘤细胞通过自噬从细胞外的新生血管中获得营养物质。非特异性抑制自噬最后阶段的药物如氯喹衍生物未必如所希望的那样有益。
她说:目前面临的挑战是了解这些不同的自噬过程的机体分子机制,确定促癌信号途径的具体靶点,同时又不影响肿瘤抑制途径。
Czyzyk-Krzeska说:当前转移性肾癌治疗主要为抑制血管生成,但抑血管生成疗法通常只延长患者几个月的生存期。我们希望这项新的研究为开发新的更有效的治疗方法铺平道路。

doi:10.1016/j.ccr.2012.02.019
PMC:
PMID:
VHL-Regulated MiR-204 Suppresses Tumor Growth through Inhibition of LC3B-Mediated Autophagy in Renal Clear Cell Carcinoma
Olga Mikhaylova, Yiwen Stratton, Daniel Hall, Emily Kellner, Birgit Ehmer, Angela F. Drew, Catherine A. Gallo, David R. Plas, Jacek Biesiada, Jarek Meller, et al.
The von Hippel-Lindau tumor-suppressor gene (VHL) is lost in most clear cell renal cell carcinomas (ccRCC). Here, using human ccRCC specimens, VHL-deficient cells, and xenograft models, we show that miR-204 is a VHL-regulated tumor suppressor acting by inhibiting macroautophagy, with MAP1LC3B (LC3B) as a direct and functional target. Of note, higher tumor grade of human ccRCC was correlated with a concomitant decrease in miR-204 and increase in LC3B levels, indicating that LC3B-mediated macroautophagy is necessary for RCC progression. VHL, in addition to inducing endogenous miR-204, triggered the expression of LC3C, an HIF-regulated LC3B paralog, that suppressed tumor growth. These data reveal a function of VHL as a tumor-suppressing regulator of autophagic programs.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#特异性#
31
#cancer cell#
28
#CEL#
32
#细胞癌#
33
#Cell#
45