Obstet Gynecol:肥胖的经产妇女性尝试顺产可以降低新生儿发病率
2015-10-20 Mechront 译 MedSci原创
研究者对47,372名可经阴道分娩的肥胖女性(BMI≥30)进行了回顾性研究,纳入的研究对象均在满月后(≥37周)分娩单胎活产婴儿。前次剖宫产、先天性畸形、死胎等排除在外。研究者分析了不同分娩方式的母儿结局,以及按产次对研究对象进行分层分析。孕产妇结局指标包括:重症监护、死亡、出血、输血或血栓栓塞。新生儿结局指标有:重症监护、死亡、癫痫发作、使用呼吸机、产伤或窒息。研究者通过泊松回归分析数据。研究
研究者对47,372名可经阴道分娩的肥胖女性(BMI≥30)进行了回顾性研究,纳入的研究对象均在满月后(≥37周)分娩单胎活产婴儿。前次剖宫产、先天性畸形、死胎等排除在外。研究者分析了不同分娩方式的母亲和新生儿的结局,以及按产次对研究对象进行分层分析。孕产妇结局指标包括:重症监护、死亡、出血、输血或血栓栓塞。新生儿结局指标有:重症监护、死亡、癫痫发作、使用呼吸机、产伤或窒息。研究者通过泊松回归分析数据。
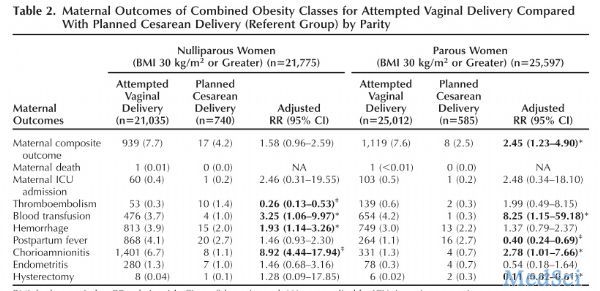
研究结果显示,15,268名尝试阴道分娩的初产妇,其成功率为 72.6% ,对于23,426名尝试经阴道分娩的经产妇,成功率为93.7%。对于初产妇,孕产妇的不良结局在尝试阴道分娩与计划性剖腹产组间,发生率无显著差异(7.7% vs 4.2% [sRR 1.58, 95% CI 0.96-2.59]) ,但是对于经产妇,该差异显著 (7.6% vs 2.5% [aRR 2.45, 95% CI 1.23-4.9)])。
新生儿不良结局发生率则刚刚相反,经产妇尝试阴道分娩,其婴儿不良结局更少(6.0% vs 11.6% [aRR 0.65, 95% CI 0.51-0.83]),但是在初产妇组该结论不成立 (10.2% vs 12.4% [aRR 0.91, 95% CI 0.74-1.12]) 。
研究结果表明,肥胖初产妇尝试阴道分娩并不会增加母儿不良反应发生率或发病率。但是对于肥胖的经产妇,尝试阴道分娩会增加孕产妇发病率,但是可以降低新生儿发病率。
原始出处:
Clark-Ganheart CA, Reddy UM,et al.Pregnancy Outcomes Among Obese Women and Their Offspring by Attempted Mode of Delivery.Obstet Gynecol. 2015 Oct 5.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#NEC#
0
#TET#
23
#发病率#
0