Biomaterials:超级自然杀伤细胞可以杀灭淋巴结转移的肿瘤细胞!
2015-11-13 MedSci MedSci原创
纽约伊萨卡康奈尔大学的研究人员在 Biomaterials杂志上揭示了他们研究和检测他们的“超级自然杀伤细胞”的过程。Michael R. King骄傲地说:“但愿以后再也看不到肿瘤细胞淋巴结转移的出现。”
纽约伊萨卡康奈尔大学的研究人员在 Biomaterials杂志上揭示了他们研究和检测他们的“超级自然杀伤细胞”的过程。Michael R. King骄傲地说:“但愿以后再也看不到肿瘤细胞淋巴结转移的出现。”
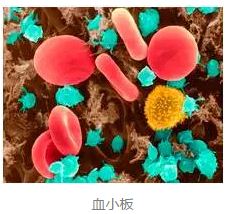
自然杀伤细胞是NK细胞的简称。它不同于T、K细胞,对靶细胞杀伤时既不需特异性抗体参加,也不需抗原预先致敏。主要存在于外周血、脾脏和骨髓中,能立即发挥非特异性杀伤靶细胞的作用,尤其是对多种肿瘤细胞有迅速杀伤和溶解作用。
King教授和他的同事们发现,通过添加一种叫做TRAIL的蛋白质(重组人肿瘤坏死因子相关凋亡诱导配体),可显著提高自然杀伤细胞这种功能,从而把它们变成“超级自然杀伤细胞”。这些“超级自然杀伤细胞”通过将TRAIL蛋白质注入肿瘤细胞中,进而导致细胞的死亡和溶解。
既往研究表明,在机体血液中的白细胞中加入TRAIL蛋白质可以杀死进入血液中的肿瘤细胞,并阻止它们转移到肺、肾、肝和其他器官。
然而,大多数肿瘤细胞会转移到淋巴结,并引起机体出现其他疾病。一旦肿瘤细胞转移至淋巴结,则患者生存的几率大大降低。
在这项研究中,King教授和他的同事们发现,他们将含有TRAIL蛋白质的脂质体注入小鼠的自然杀伤细胞中,小鼠的自然杀伤细胞会杀死淋巴结附近的肿瘤细胞。这些“超级自然杀伤细胞”在几天内便可消灭小鼠体内的肿瘤细胞。
脂质体是微小的球形囊封闭式薄膜,可以用作提供药物和营养细胞的中介或传媒。
King教授说道:“在我们的研究中,我们使用脂质体纳米粒子,这些脂质体纳米粒子中含有TRAIL蛋白质,将含有TRAIL蛋白质的脂质体纳米粒子注入自然杀伤细胞中,我们便称之为‘超级自然杀伤细胞’,然后这些“超级自然杀伤细胞”便可完全消除小鼠淋巴结处转移的肿瘤细胞。”教授和他的同事打算几年后进行人体试验。
淋巴结是肿瘤转移和进展的重要通路。在早期阶段中,肿瘤很小且局限,癌细胞还没有扩散到淋巴结。在第二和第三期中,肿瘤变得更大,可能扩散入淋巴结。第四期,癌症细胞转移至淋巴结和身体其他部位。因此,若“超级自然杀伤细胞”得以成功研制,并应用于人体,则肿瘤患者治愈有很大希望,他们生存的几率会更高。
原始出处:
Siddarth Chandrasekaran et al.,Super natural killer cells that target metastases in the tumor draining lymph nodes, Biomaterials, 2 Nov,2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Biomaterials#
36
#Bio#
27
#淋巴结#
27
#淋巴结转移#
34
#肿瘤细胞#
27
#自然杀伤细胞#
37