Sci Transl Med:术后贴一片,复发转移靠边站!科学家发明“免疫凝胶”,或可大幅降低术后癌症复发转移风险
2018-04-08 姬亚茹 奇点网
对付恶性肿瘤,手术切除无疑是最主要的治疗方法,然而将肿瘤"一刀切"并非万全之策,无法清除的残留癌细胞”生根“后又会形成星火燎原之势。据悉,术后5年内有40%癌症患者复发,90%患者因此死亡。
对付恶性肿瘤,手术切除无疑是最主要的治疗方法,然而将肿瘤"一刀切"并非万全之策,无法清除的残留癌细胞”生根“后又会形成星火燎原之势。据悉,术后5年内有40%癌症患者复发,90%患者因此死亡。
免疫凝胶
癌症术后治疗面临的问题
此前有研究报道,术后伤口愈合对肿瘤复发和转移起到了推波助澜的作用,形成的免疫抑制微环境不仅帮助癌细胞转移、侵袭和增殖,还抑制了抗肿瘤免疫细胞活性,与此同时,免疫系统将大部分精力集中在愈合手术伤口,降低了对癌细胞的防范能力。
虽然临床上已有癌症免疫疗法来解决这一问题,但反应率有待提高,而且对于有乳腺癌来说,大多数治疗药物,甚至是免疫疗法效果甚微,那么有没有可能开发出一个适用人群范围更广的免疫疗法呢?
哈佛大学医学院的研究人员注意到,之前有研究显示,与全身给药相比,在肿瘤原发部位给药是一种安全有效的方法,既可以打破局部的免疫耐受,又能够产生全身抗肿瘤免疫,从而避免引发严重的不良反应。
据此,科学家们便萌生了一个想法:在肿瘤切除部位缓慢释放药物调节免疫抑制微环境,以达到预防肿瘤复发并消除转移的目的。
神奇的水凝胶
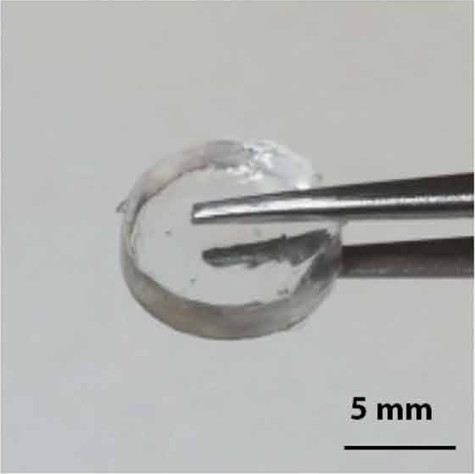
而使用透明质酸制作的水凝胶支架既可以达到缓慢释放药物的效果,又对人体无害(天然存在人体中),还能提高T细胞治疗的有效性。这种生物材料便成了科学家们的首选。
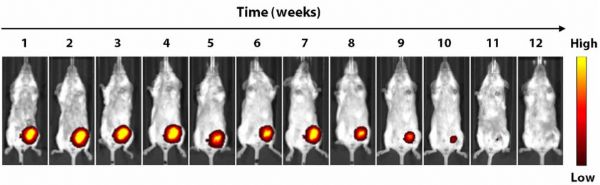
于是,研究人员制备了水凝胶支架并验证了它的稳定性和生物相容性,将水凝胶支架进行荧光标记后,放置在乳腺癌小鼠肿瘤切除部位,发现它可在5周内开始降解,12周内完全吸收。同时放置在非肿瘤小鼠中第12小时和15周后发现小鼠的植入部位没有异常。
水凝胶支架在乳腺癌切除小鼠模型中,5周内开始降解,12周内完全吸收
接着,研究人员进一步验证了水凝胶支架的释放特性。Cy7-CA是一种荧光团,其物理性质与本实验中使用的化合物R848非常相似。他们将该荧光团装载在溶液或水凝胶支架中,并放置在非肿瘤小鼠模型中发现,溶液中的荧光团2小时内信号丢失60%,而在水凝胶支架中24小时后才能检测到信号衰减, 在这段时间里水凝胶支架释放的荧光素信号比溶液中高3倍,明显延长了药物释放。
同时分析发现,水凝胶支架不会与抗体、细胞因子和小分子发生反应致其失活。
既然水凝胶支架稳定性良好且具有高度的生物相容性,又能延长药物的释放,但装载哪种药物能最有效地预防肿瘤的复发和转移呢?
水凝胶上的药
为此,研究人员将水凝胶装载几种免疫调节化合物如抗体(抗PD-1,抗CTLA-4),细胞因子(IL-15sa)和小分子物质(雷利度胺、塞来昔布、STING-RR和R848),并将其放置在乳腺癌小鼠肿瘤切除部位,每周检测肿瘤负荷。三个月后发现,水凝胶装载的STING-RR或R848(免疫凝胶)最有效地预防了肿瘤复发,并消除了肺转移灶。没有放置水凝胶小鼠存活率不到10%,而装载R848的水凝胶可使小鼠存活率达到70%以上。
这里简单介绍下STING-RR和R848,STING(干扰素基因刺激因子)激动剂STING-RR可刺激肿瘤部位的树突细胞产生干扰素β(IFN-β),启动T细胞引发抗肿瘤免疫应答;而R848是Toll样受体7/8激动剂,通过树突细胞诱导I型IFNs和共刺激分子的表达,通常被用作疫苗佐剂或作为病毒或肿瘤性皮肤病变的局部疗法。
为什么“免疫凝胶"会预防肿瘤复发并消除肺转移呢?研究人员对乳腺癌切除术后放置免疫凝胶的小鼠模型分析发现,脾脏和肺中NK细胞和树突细胞增多且被激活(表达了CD40和CD86以及MHCⅡ),增多的树突细胞诱导了强大的系统性抗肿瘤免疫反应(CD4+T细胞和CD8+T增多,中央记忆体数量增加)。因此,免疫凝胶延长释放先天性免疫激动剂,招募了大量的树突细胞,并将肿瘤抗原提呈给免疫细胞,增强了对癌细胞的免疫应答。
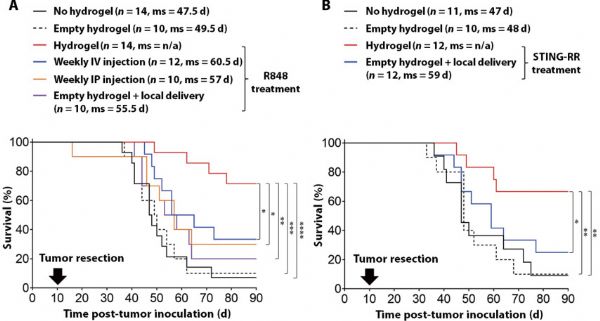
如果离开了水凝胶的环境,单独使用上面这两种先天免疫激动剂是否也能发挥同样的效果呢?研究人员比较了单独使用水凝胶、每周静脉注射、腹腔注射和局部注射药物后效果发现,这两种药物仅装载在水凝胶支架中才能显着改善小鼠的存活率。
与静脉注射、腹腔注射和局部注射相比,水凝胶装载R848和STING-RR显着提高了小鼠的存活率
同时,研究人员进一步发现,这种“免疫凝胶”在临床的实用性及安全性较强,它可在4℃的环境下保存一周,也不会对血液成分和肝肾功能产生影响。
适用于多种肿瘤
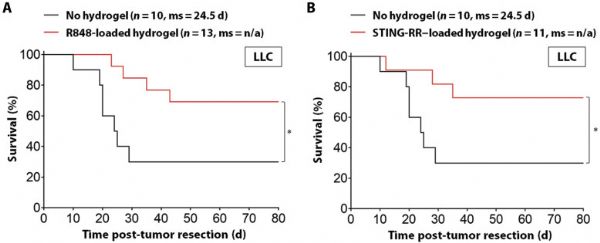
令人欣喜的是,这种“免疫凝胶”不仅在乳腺癌切除后小鼠模型中有效,在肺癌和黑色素瘤切除后小鼠模型中也可提高小鼠存活率,在肺癌模型中,免疫凝胶使小鼠近3个月存活率提高到70%左右,无免疫凝胶的小鼠存活率仅有近30%。
围手术期使用免疫凝胶显着延长肺癌小鼠存活率
哈佛大学医学院助理教授Michael Goldberg博士认为,“免疫凝胶”创造了一个促使免疫细胞长期攻击肿瘤的微环境,与目前的肿瘤免疫疗法相比,这种免疫凝胶适用的人群范围更广,任何实体瘤切除的手术患者都可能从中受益。
原始出处:Park, C.G., et al., Extended release of perioperative immunotherapy prevents tumor recurrence and eliminates metastases. Sci Transl Med, 2018. 10(433).
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#转移风险#
38
#Transl#
24
#TRA#
24
#癌症复发#
34
#凝胶#
37
#Med#
32