上海全面停止使用三价脊髓灰质炎减毒活疫苗
2016-08-30 上海卫生计生委网站 上海卫生计生委网站
经国务院同意,自2016年5月1日起我国实施新的脊髓灰质炎(以下简称“脊灰”)疫苗免疫策略,停用三价脊灰减毒活疫苗(tOPV),用二价脊灰减毒活疫苗(bOPV)替代tOPV,并将脊灰灭活疫苗(IPV)纳入国家免疫规划。调整脊灰疫苗免疫策略是全球最终实现消灭脊灰目标的重要步骤,新策略的实施既有助于减少脊灰减毒活疫苗所致的相关病例的发生,同时也可有效降低脊灰野病毒输入和传播风险。根据国家统一部署,结合
经国务院同意,自2016年5月1日起我国实施新的脊髓灰质炎(以下简称“脊灰”)疫苗免疫策略,停用三价脊灰减毒活疫苗(tOPV),用二价脊灰减毒活疫苗(bOPV)替代tOPV,并将脊灰灭活疫苗(IPV)纳入国家免疫规划。调整脊灰疫苗免疫策略是全球最终实现消灭脊灰目标的重要步骤,新策略的实施既有助于减少脊灰减毒活疫苗所致的相关病例的发生,同时也可有效降低脊灰野病毒输入和传播风险。
根据国家统一部署,结合本市实际,自2016年5月1日起本市全面实施脊髓灰质炎序贯免疫程序(即2月龄、3月龄各接种1剂次IPV,4月龄、4周岁各接种1剂次bOPV),并全面停止使用tOPV。本市各相关医疗卫生机构在2016年5月15日前将按照要求对本市范围内所有tOPV进行清点、回收和封存,并由市、区县疾病预防控制中心予以集中统一销毁。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






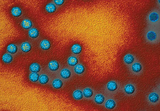




#活疫苗#
30
很好,不错,以后会多学习
52
#脊髓灰质炎#
43
继续关注
56
继续学习
68
继续关注
54
阅读了。
51