JAMA:乳腺癌的ERBB2 (HER2) 检测病例问答,来试试?
2016-03-28 MedSci MedSci原创
女性,35岁,因左侧乳房肿块就诊于社区医院。乳房射线提示2个孤立的包块:3点钟方向1.4cm,距乳头10cm;乳房外侧一个1.3cm的肿块,距乳头4cm。腋窝超声提示淋巴结肿大,细针穿刺细胞学为恶性细胞。图像引导的两个肿块粗针活检提示低分化浸润性导管腺癌。雌激素受体(ER)在95%的肿瘤细胞显示强阳性,孕激素受体(PR)在不到5%的肿瘤细胞为阳性,免疫组化(IHC)示人类表皮生长因子受体2(ERB
女性,35岁,因左侧乳房肿块就诊于社区医院。
乳房射线提示2个孤立的包块:3点钟方向1.4cm,距乳头10cm;乳房外侧一个1.3cm的肿块,距乳头4cm。腋窝超声提示淋巴结肿大,细针穿刺细胞学为恶性细胞。图像引导的两个肿块粗针活检提示低分化浸润性导管腺癌。雌激素受体(ER)95%强阳性,孕激素受体(PR)5%阳性,免疫组化(IHC)示人类表皮生长因子受体2(ERBB2(HER2))为1+。(如表)
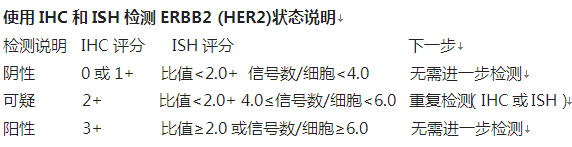
来自美国临床肿瘤协会和美国病理学家协会指南
你怎么理解这些检测结果?
A、患者是ERBB2 (HER2)阴性乳腺癌
B、患者是ERBB2 (HER2)阳性乳腺癌
C、结果可疑,需重新检测
D、结果的组织病理学不一致
答案:D
ERBB2(HER2)(第二个发现的人类表皮生长因子受体)是所有诊断为乳腺癌患者的最重要参数之一。在17号染色体上HER2基因发生扩增和或/在15%-20%的原位乳腺癌患者上有HER2蛋白过度表达。这导致细胞增殖,促进血管再生,提高了细胞生存路径,从而增加了肿瘤生物学的侵袭性,导致更差的预后。ERBB2(HER2)检测可以识别出能从ERBB2(HER2)靶向治疗(如曲妥珠单抗和帕妥珠单抗)受益更多的患者,抑制ERBB2(HER2)驱动细胞机制,显著改善生存率。组织病理学的不一致性出现在当低级别分化良好的肿瘤表现出ERBB2(HER2)阳性或组织学上高级别分化不良的肿瘤有ERBB2(HER2)阴性结果时。
适用于ERBB2(HER2)检测的定义
1.可疑结果
根据ASCO/CAP指南的IHC或ISH结果既不是阳性也不是阴性。此时应重复检测(IHC或ISH)。
2.组织病理学不一致
结果显示高级别肿瘤ERBB2(HER2)阴性,或特殊类型(如纯粘液性或筛状癌)的低级别肿瘤ERBB2(HER2)阳性。
3.瘤内非均质性结果
在同一个肿瘤不同区域出现ERBB2(HER2)阳性和阴性结果。与粗针穿刺不同,这可见于手术切除的有形态学区别的肿块。
治疗
这个病人的肿瘤是低分化的,但ERBB2(HER2)阴性,暗示了组织病理学的不一致性。考虑到她肿块的多发,进行了改良乳腺切除术,切除样本使用ISH进行了ERBB2(HER2)检测。结果显示ERBB2(HER2)/CEP17比例为4.6,20个细胞中有267个ERBB2(HER2)信号,阳性结果,使她具有了使用曲妥珠单抗和帕妥珠单抗靶向治疗的资格。
可选择的诊断测试方法?
IHC和ISH是目前许可的评估原位乳腺癌ERBB2(HER2)状态的唯一方法。
病人的结局
最后手术确定为多灶性浸润性导管癌,累及5/14个腋窝淋巴结。接受了6个周期的多烯紫杉醇,卡铂,曲妥珠单抗,和帕妥珠单抗辅助治疗,之后进行了3个月的曲珠单抗完成1年的治疗目标。伴随化疗进行了激素辅助疗法和局部放疗。诊断后1年的临床评价显示无复发迹象。
临床要点
1.ERBB2(HER2)检测可识别具有侵袭性的和预后较差的肿瘤,但这些病人可从靶向治疗中显著获益并极大的提高生存。
2.无单一标准检测肿瘤组织的ERBB2(HER2)状态,但目前支持的两种检测方法是IHC和ISH。
3.但初次检查结果可疑时,应重复检测使用IHC或ISH。
4.IHC用于检测细胞表面蛋白质表达,ISH用于检测基因扩增。
原始出处:
Talal Hilal, MD1; Edward H. Romond, MD2 ERBB2 (HER2) Testing in Breast Cancer ,
JAMA. 2016;315(12):1280-1281. doi:10.1001/jama.2015.17463.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ErbB2#
35
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
61
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
52
非常好!
65
值得学习
109