NEJM:非洲蜱叮咬热-病例报道
2019-03-07 xing.T 网络
非洲蜱叮咬热是由非洲立克次体引起的,并且由大壁虱属的蜱传播,其喂养模式导致旅行组内的多个焦痂和聚集的病例。经验性地加入强力霉素治疗,并且在24小时内两个孩子的发热都得到了解决。
患者为10岁和12岁的两个兄弟,从南非莫桑比克和赞比亚旅行返回后,均因发烧和头痛2天而就诊。他们没有报告任何蜱叮咬。
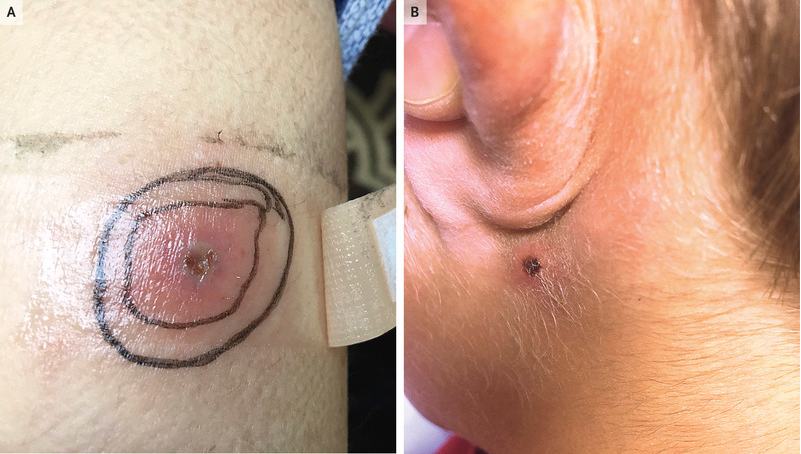
在检查时,哥哥小腿上有焦痂(如图A所示),而弟弟在耳后(如图B所示)和眉毛上有焦痂。两兄弟在手腕、腿部和躯干上都有一个无咬痕、斑状突起的皮疹,以及与皮肤相邻的区域性淋巴结病。疟疾涂片和血培养均为阴性。推测蚊虫叮咬而启动阿莫西林-克拉维酸治疗;然而,多处焦痂以及两名家庭成员受到影响的事实引起了对非洲蜱叮咬发热的怀疑。
非洲蜱叮咬热是由非洲立克次体引起的,并且由大壁虱属的蜱传播,其喂养模式导致旅行组内的多个焦痂和聚集的病例。经验性地加入强力霉素治疗,并且在24小时内两个孩子的发热都得到了解决。
给予强力霉素7天,焦痂在治疗开始后2周内消除。最初为阴性的立克次体血清学检查在3个月后的随访中均为阳性。
原始出处:
Ines Mack,et al.African Tick-Bite Fever.N Engl J Med 2019;https://www.nejm.org/doi/full/10.1056/NEJMicm1810093
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#蜱#
37
谢谢分享,学习了
83
谢谢分享,学习了
78