NEJM:膝关节镜术后或小腿石膏固定后抗凝治疗能预防血栓吗?
2016-12-04 xing.T MedSci原创
在膝关节镜手术后预防性的使用8天的低分子肝素或小腿石膏固定后全程使用低分子肝素并不能有效的预防有症状性静脉血栓形成。
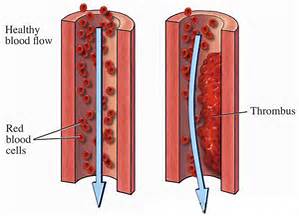
膝关节镜术后或小腿石膏固定后预防血栓形成治疗来预防临床上明显的静脉血栓栓塞是存在争议的。近日,顶级医学期刊NEJM上发表了一篇研究文章,研究人员比较了那些接受抗凝治疗和那些没有接受抗凝治疗患者在膝关节镜术后或小腿石膏固定后有症状性静脉血栓栓塞的发生率。
研究人员进行了两个平行的、实用的、多中心、随机、对照、公开分组但进行盲法结果评估的试验:POT-KAST试验,该研究纳入的是接受膝关节镜手术的患者;POT-CAST试验,该研究纳入的是小腿石膏固定治疗的患者。这些患者被随机分配接受预防剂量的低分子量肝素(POT-KAST试验的患者膝关节镜术后8天使用;POT-CAST试验的患者石膏固定全程使用)或无抗凝治疗。主要结局事件为膝关节镜术后或小腿石膏固定后3个月内有症状的静脉血栓栓塞和大出血的累积发生率。
在POT-KAST试验中,共纳入了1543例患者进行随机分组,其中1451例纳入意向治疗人群。在治疗组,静脉血栓栓塞发生为731例参与者中有5例(0.7%);在对照组为720例参与者中有3例(0.4%)(相对风险为1.6;95%可信区间为0.4至6.8;风险绝对差异为0.3个百分点;95%可信区间为-0.6至1.2)。在治疗组中大出血有1例(0.1%);在对照组中有1例(0.1%)(风险绝对差异为,0个百分点;95%可信区间为-0.6至0.7)。
在POT-CAST试验中,共纳入了1519例患者进行随机分组,其中1435例纳入意向治疗人群。在治疗组中,静脉血栓栓塞发生为719例参与者有10例(1.4%);在对照组中为716例参与者有13例(1.8%)(相对风险为0.8;95%可信区间为0.3至1.7;风险绝对差异为-0.4个百分点;95%可信区间为-1.8至1),未发生大出血事件。在这两项试验中,最常见的不良事件是感染。
该研究结果表明,在膝关节镜手术后预防性的使用8天的低分子肝素或小腿石膏固定后全程使用低分子肝素并不能有效的预防有症状性静脉血栓形成。
原始出处:
Raymond A. van Adrichem, et al. Thromboprophylaxis after Knee Arthroscopy and Lower-Leg Casting. NEJM. December 3, 2016.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#膝关节镜#
27
文章不错,值得学习
56
学习了,但怎样才有效呢?
58
要有了解哦!
45
DVT应该引起重视
42
#关节镜#
32
谢谢,学习了
56