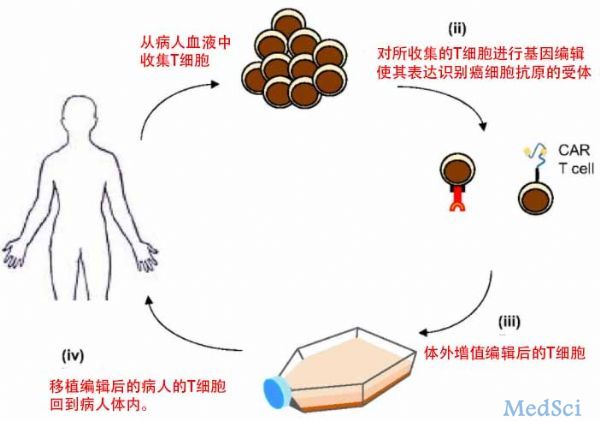
Nature:用CRISPR/Cas9技术将肿瘤抗原受体编辑进T细胞TRAC基因位点,增强杀死癌细胞的能力
2017-03-09 LEO.C MedSci原创
运用CRISPR/Cas9编辑的CAR-T细胞对于急性淋巴细胞白血病(Acute lymphoblastic leukemia)有更好的疗效。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肿瘤抗原#
34
#CRISPR/Cas9技术#
32
#Nat#
35
#TRA#
37
#基因位点#
26
#RISPR/Cas9#
38
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。
51
#癌细胞#
27
#CRISPR#
33
#CRISPR/Cas9#
38