MMWR:在B.1.617.2(Delta)和B.1.1.529(Omicron)变异优势时期住院的经实验室确认的SARS-CoV-2感染成人的临床特征和转归
2022-03-20 从医路漫漫 MedSci原创
2021年12月中旬,引起新冠肺炎的SARS-CoV-2的B.1.1.529(欧米克隆)变异株超过B.1.617.2(德尔塔)变异株,成为加利福尼亚州的主要毒株。

背景:2021年12月中旬,引起新冠肺炎的SARS-CoV-2的B.1.1.529(欧米克隆)变异株超过B.1.617.2(德尔塔)变异株,成为加利福尼亚州的主要毒株。初步报告表明,欧米克隆变异株传播性更强,对疫苗中和具有抵抗力,但与以前的变异株相比,造成的疾病不那么严重。
方法:为了描述在德尔塔和奥美康优势时期住院的非典型肺炎冠状病毒2型患者的特征,回顾性地从加利福尼亚州洛杉矶一家学术医院2021年7月15日-9月23日(德尔塔优势时期)和2021年12月21日-2022年1月27日(奥米康优势时期)收治的≥18岁患者的电子健康记录(EHR)中提取临床特征和转归,这些患者的反转录-聚合酶链反应(RT-PCR)SARS-CoV-2检测结果为阳性(Omicron优势时期为2021年7月15日-9月23日)和2022年12月21日-2022年1月27日(奥米康为优势时期)。
结果:与三角洲优势时期的患者相比,在奥美康优势时期入院的成年人接受了新冠肺炎初级疫苗系列的最后一剂疫苗(完全接种)的比例较高(39.6%对25.1%),接受新冠肺炎指导治疗的较少。尽管在奥美康(Omicron)占优势期间,重症监护病房(ICU)入院和有创机械通气(IMV)所需的人数较少,住院期间死亡的人数也较少,但按接种状况分层后,ICU入院或有创机械通气(IMV)的情况没有显著差异。完全接种Omicron期患者住院期间死亡的人数(3.4%)比Delta期患者(10.6%)要少。在奥米克隆期患者中,接种疫苗与入住重症监护病房的可能性较低有关,而在65岁的≥患者中,住院期间死亡的可能性较低。在接受强化剂量的成年人中,入住ICU和死亡的可能性最低。在最初的Omicron期住院治疗中,19.8%的患者被临床评估为非新冠肺炎疾病入院,与被认为可能因新冠肺炎而入院的成年人相比,这些患者更年轻(中位年龄为38岁对67岁),更有可能接受过至少一剂新冠肺炎疫苗(84.6%对61.0%)。虽然在奥美康流行期间,20%的与SARS-CoV-2相关的住院可能是由非新冠肺炎疾病推动的,但大量的住院给卫生系统带来了压力。

图 在奥米克龙变异流行期间,737名患有sars-cov-2感染的成人在重症监护病房入院、使用有创机械通气和住院期间死亡,按年龄组和疫苗接种状态分类*
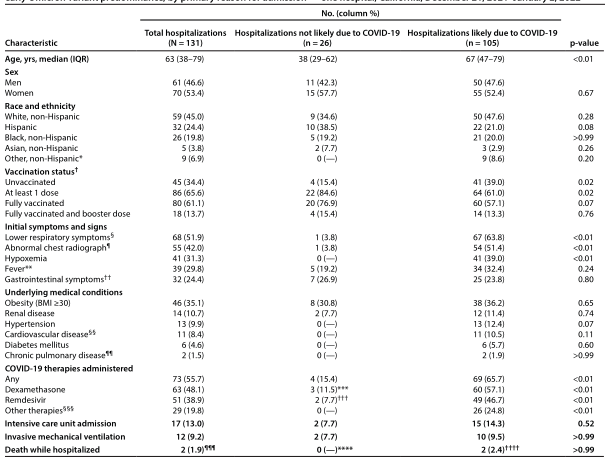
表2.131名成人在Omicron变异早期感染SARS-CoV-2的人口统计学、临床特征和临床结果
结论:疫苗接种,包括为那些完全接种疫苗的人增加剂量,对于最大限度地减少感染SARS-CoV-2的成年人出现严重健康后果的风险仍然至关重要。
原文出处: Modes ME, Directo MP, Melgar M, et al.Clinical Characteristics and Outcomes Among Adults Hospitalized with Laboratory-Confirmed SARS-CoV-2 Infection During Periods of B.1.617.2 (Delta) and B.1.1.529 (Omicron) Variant Predominance - One Hospital, California, July 15-September 23, 2021, and December 21, 2021-January 27, 2022.MMWR Morb Mortal Wkly Rep 2022 Feb 11;71(6)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CRO#
44
#SARS-CoV#
50
#临床特征#
46
#Micro#
35
学习了,谢谢分享
44
#SARS#
28
#变异#
28