European Radiology:消融和腹腔镜肾部分切除术在治疗T1肾细胞癌方面的远期疗效
2022-08-16 shaosai MedSci原创
由于影像学引导下的消融(IGA)具有微创性,而且与PN相比,理论上能够保留肾功能并降低并发症发生率,因此在SRMs的治疗中采用的比例迅速增加。
传统上,患有体积小的肾脏肿块(SRMs)的患者可通过根治性或部分肾切除术(PNs)进行治疗。然而临床上,腹腔镜肾切除术(LPN)有很大程度的并发症发生率(约20%)。1997年首次报道了经皮图像引导的射频消融(RFA)在SRMs中的应用。由于影像学引导下的消融(IGA)具有微创性,而且与PN相比,理论上能够保留肾功能并降低并发症发生率,因此在SRMs的治疗中采用的比例迅速增加。
目前欧洲泌尿外科协会(EAU)的指南表明,对T1期肾脏肿块进行PN治疗的证据十分充分,而只对那些有明显合并症和虚弱的人提供IGA的证据并不充分。另一方面,美国泌尿外科协会(AUA)指南建议将热消融作为管理cT1a肿瘤的替代方法,但强调缺乏高质量的文献支持。AUA指南也明确指出了长时间随访的重要性(>5年),以准确评估晚期局部复发。
近日,发表在European Radiology杂志的一项研究提供了本机构10年的经验和证据,为接受影像学引导的CRYO或RFA和LPN治疗活检或组织学证实的T1aN0M0和T1bN0M0肾细胞癌(RCC)患者的长期肿瘤学预后提供了临床指导。

本项回顾性队列研究的研究对象为2003年-2016年在本机构接受冷冻消融(CRYO)、射频消融(RFA)或LPN的局部RCC(T1a/bN0M0)患者。使用Cox回归和log-rank分析比较了肿瘤学预后,并使用Kruskal-Wallis和Wilcoxon-rank检验比较了eGFR变化。
共确定了296名(238名T1a,58名T1b)连续患者;103名、100名和93名患者分别接受了CRYO、RFA和LPN。中位随访时间分别为75、98和71个月。在单变量分析中,CRYO、RFA和LPN的所有肿瘤学结果都具有可比性(P>0.05)。在多变量分析中,与LPN相比,接受RFA的T1a患者的无局部复发生存期(LRFS)(HR 0.002,95% CI 0.00-0.11,p = 0.003)和无转移生存期(HR 0.002,95% CI 0.00-0.52,p = 0.029)有所改善。在T1a和T1b患者中,CRYO(HR 0.07,95% CI 0.01-0.73,p = 0.026)和RFA(HR 0.04,95% CI 0.03-0.48,p = 0.011)的LRFS率都有改善。与LPN相比,接受CRYO和RFA的患者术后eGFR的中位数下降明显较小(T1a:p < 0.001;T1b:p = 0.047)。
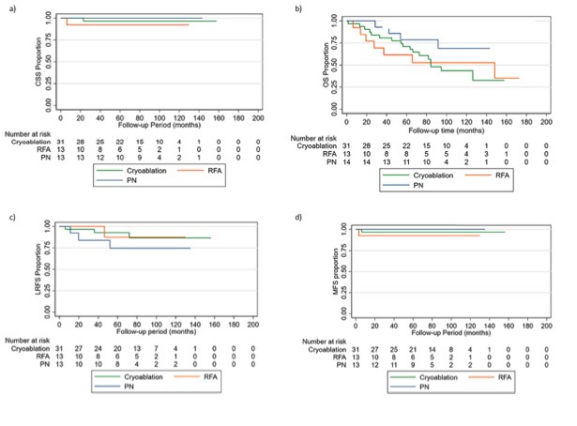
图 T1b 患者a 癌症特异性生存率、b 总生存率、c 无局部复发生存率和 d 无转移生存率
本研究表明,IGA在肿瘤学预后方面与LPN的效果一致,且IGA在肾脏功能保护方面明显优于LPN。
原文出处:
Vinson Wai-Shun Chan,Filzah Hanis Osman,Jon Cartledge,et al.Long-term outcomes of image-guided ablation and laparoscopic partial nephrectomy for T1 renal cell carcinoma.DOI:10.1007/s00330-022-08719-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
41
#远期疗效#
48
#细胞癌#
41
#切除术#
40
#腹腔镜#
51
#消融#
47