1.患者基本信息:
男,64岁
主诉:便血伴肛门下坠5月余。
体格检查:腹平软,全腹无明显压痛及反跳痛,未及包块,肝脾肋下未及
指检:距肛门8cm可触及环形肿物,绕肠一周,质硬,基底部活动度差
ECOG评分:0分。活动能力完全正常
BMI:25.2kg/m2
实验室检查:CEA:44.64ng/ml,CA199:701U/ml
2. 距肛缘10-16cm直肠可见环周生长不规则新生物,上覆污苔,边缘隆起,管腔呈中心性狭窄,内镜尚可通过,取6块送检。
诊断:直肠癌 病理:(直肠)腺癌
3.病变距肛门约8cm,病变长度约46mm,病变沿管壁浸润性生长,肠腔不规则、变窄,病变边界不清,达浆膜面致浆膜面模糊,直肠系膜内见结节状淋巴结影。
诊断:直肠癌(累及浆膜面、直肠系膜,区域淋巴结肿大、骶前筋膜增厚)
4.肝脏MRI增强检查发现:
肝脏多发病灶,分散在右肝,较大者约4.5*4.3 cm,考虑为转移
5. 患者基本情况总结:
男,64岁
ECOG评分:0分
BMI:25.2kg/m2
距肛门8cm环形肿物,质硬,活动度差
实验室检查:CEA:44.64ng/ml,CA199:701U/ml
诊断:直肠癌肝转移(cTNM:T3-4aN+M1a)
Kras/Nras 突变,MSS,PD-1阴性
多发性肝转移
6.肝脏是结直肠癌转移的特异性器官
有15-25%结直肠癌患者在确诊时即合并有肝转移,
另有15-25%患者在结直肠癌原发灶根治术后可发生肝转移,其中绝大多数(80%-90%)的肝转移灶初始无法获得根治性切除。
晚期结直肠癌肝转移发生率>80%,患者死因的2/3是归因于肝转移。
未经治疗的肝转移患者的mOS仅6.9个月,无法切除患者的5yOS <5%,而肝转移灶完全切除达到NED(no evidence of disease, NED)状态患者的mOS为35个月, 5yOS 为30%-57%。
努力达到NED (no evidence of disease, NED),
是我们永远的追求!
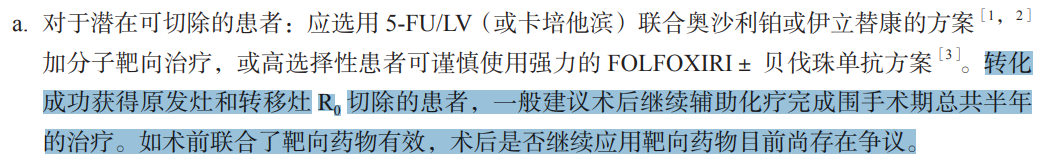
7.潜在可切除的治疗分层
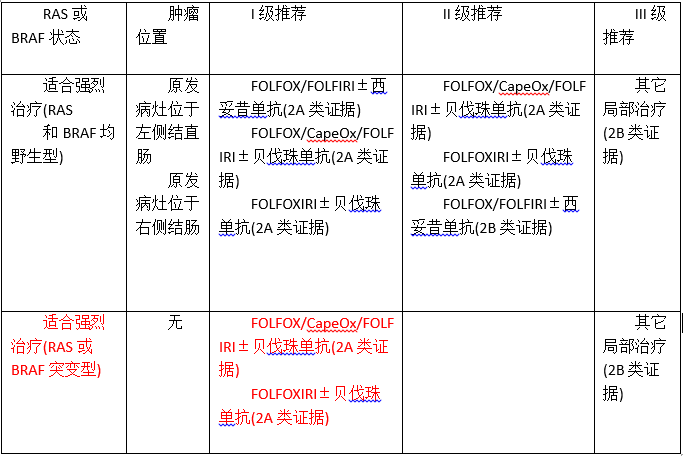
8. 治疗方案
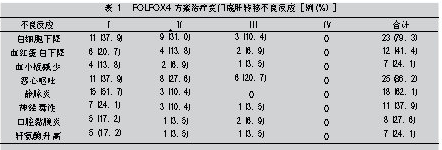
2021年4月20日-2021年8月15日,
行标准“FOLFOX+贝伐珠单抗”方案,化疗6个周期
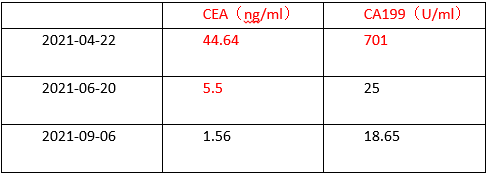
9. 治疗后肿瘤标记物对比
10. 手术治疗:
2021年9月9日行腹腔镜下直肠癌根治术(Dixon)+回肠预防性造口术,术后6天痊愈出院
11. 术后病理结果:
直肠隆起型中-高分化腺癌(化疗后标本),侵出外膜。上下断端净。
淋巴结 (0/17) TRG:3级
MLH1(部分+),MSH2(+)MSH6(+),PMS2部分(+),P53(80%+)
Her-2(1+),PD-L1(-)
Ki67(70%+)
术后分期:T4aN0M1a, IVa期
12. 后续治疗:
2021年9月22日
对肝脏转移灶残余行超声引导下射频消融后仍沿用术前化疗方案
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#贝伐珠#
25
#FOLFOX#
43
#贝伐#
32