PeerJ:摄入油脂品种换一换,食管癌风险竟能差4倍?4个脂肪酸模式,1种可将ESCC风险翻一番,而另1种却打对折!
2022-04-06 LILYMED MedSci原创
PeerJ:膳食脂肪酸类型与食道鳞状细胞癌的风险
根据《2020年全球癌症统计》,食管癌的发病率居全球第7位,是全球第六大癌症死亡原因。亚洲约占所有食管癌病例的78%,而49%的病例发生在中国。食管癌是中国第六大常见癌症和第四大致命癌症,年龄调整后的5年生存率相对较低,在20-30%之间,超过90%的食管癌病例是食管鳞状细胞癌(ESCC)。
ESCC的发生和预后受多种因素的影响。吸烟、饮酒和环境致癌物暴露是公认的ESCC的主要危险因素。近年来,越来越多的研究强调了营养在这种癌症中的关键作用。在营养因素中,脂肪酸在肿瘤发生中的作用越来越受到关注。目前,一些研究发现脂肪酸与各种癌症的风险密切相关,如肺癌、胰腺癌、结直肠癌和食道癌。
然而,无论是在理论上还是在经验上,由于单一营养或食物方法的局限性,膳食模式评估已成为营养流行病学中测量膳食暴露的一种替代方法。FA模式分析显示了各种脂肪酸之间的相互作用,并解释了它们与疾病的复杂关联。多种脂肪酸的组合比单一脂肪酸对ESCC风险的影响更大。因此,重要的是要考虑脂肪酸的摄入模式。目前,脂肪酸组合与发生ESCC的关联尚未被评估。因此,本研究假设不同的膳食FAPs与ESCC的风险相关,旨在明确特定的膳食FAPs,并研究产生的FAPs与ESCC之间的关系。
共招募了 422 名患者和 423 名对照。将膳食脂肪酸纳入因子分析。多变量逻辑回归和限制三次样条用于评估不同膳食脂肪酸模式(FAPs)对食管癌的特异性风险。在按生活方式暴露因素(吸烟、饮酒、腌制食品、油炸食品、热食、硬食)分层后,应用森林图显示 FAP 与 ESCC 风险之间的关联。

四个主要因子的脂肪酸因子负荷
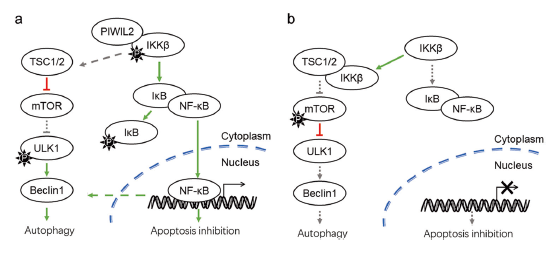
36种脂肪酸的相关矩阵如图1所示。因子分析,包括36种主要脂肪酸,确定了4个因子,解释了研究人群中这些变量的60.8%的变异。聚类分析也发现了类似的模式。提取4个FA因子评分构建膳食脂肪酸的FAP评分。根据每种模式的主要贡献者(表2),模式1组成主要包括20:0、16:0、11:0、12:0、8:0、18:0、17:0、18:1和20:2,以中链和长链饱和脂肪酸为特征(“MLC-SFA”模式)。模式2的特征是SFAs中从22:6、24:1、20:5、20:1、20:3、20:4和24:0的高正负荷;这被称为" EC-UFA "模式。研究人员将第三种FA模式定性为“SFA模式”,高因子负荷为6:0,10:0, 4:0, 13:0, 14:0和14:1。第四种模式以22:3、22:5、22:4和15:0的高正负荷为特征,称为“n-3 LC-PUFA”模式。


膳食脂肪酸评分与食物组之间的相关性
MLC-SFA 模式评分与“动物油”摄入量呈正相关(r = 0.124,P = 0.002)。EC-UFA 模式代表“花生油”含量相对较高的饮食(r = 0.189,P < 0.001)。“n-3 LC-PUFA模式”评分与“深海鱼”摄入量呈正相关(r = 0.099,P = 0.015)。
脂肪酸模式评分与 ESCC 发病率的关系
根据AIC评估模型拟合性能,模型3的AIC最低,拟合效果最好。在多变量分析中,在调整所有协变量后,n-3 LC-PUFA 模式与较低的 ESCC 可能性相关(OR:0.53, 95% CI [0.34, 0.81],P = 0.003)。在对潜在的混杂变量进行调整后,EC-UFA 模式与 ESCC 呈正相关(OR:2.07, 95% CI [1.31, 3.26],P = 0.002)。MLC-SFA 模式和 SFA 模式与 ESCC 无显着相关性(表3)。

膳食脂肪酸评分与ESCC发病率呈线性趋势
四种 FAP 的摄入量与 ESCC 风险之间的剂量反应关系如图2所示。EC-UFA 模式与 ESCC 风险之间存在非线性正相关(非线性p <0.05)。然而,n-3 LC-PUFA 模式与 ESCC 风险之间存在非线性负相关(非线性p <0.001)(图 2)。

膳食脂肪酸模式与ESCC风险的分层分析
图 3表明 FAP 与 ESCC 风险之间的关联按生活方式暴露因素分层。当按油炸食品分层时,MLC-SFA 模式与 ESCC 风险之间的关联是不同的(I 2 = 75.7%,P异质性 = 0.043)。EC-UFA 模式与 ESCC 风险之间的关联因腌制食品而异(I 2 = 78.2%,P异质性 = 0.032)。当按吸烟分层时,SFA 模式与 ESCC 风险之间的相关性发生了变化(I 2 = 99.3%,P异质性<0.001)。此外,此外,在饮酒(I 2 = 91.4%,P异质性 = 0.001)、腌制食品(I 2 = 91.4%,P异质性)和油炸食品(I 2 = 93.8%,P异质性<0.001)的人群中,观察到n-3 LC-PUFA模式与ESCC风险之间的关联存在差异。

膳食脂肪酸模式与临床病理因素的相关性
在临床病理特征中,N分期与EC-SFA模式显着相关(r s = 0.270,P < 0.001)。EC-UFA 模式的摄入量较高可能与晚期疾病的较高风险有关。M 分期与 n-3 LC-PUFA 的模式呈负相关(r s = - 0.175,P = 0.003)。然而,T 分期与 FAP 没有显着相关性。
在这项以医院为基础的病例对照研究中,确定了四种主要的膳食模式,即中长链SFA (MLC-SFA)、偶链不饱和脂肪酸(EC-UFA)、SFA和n-3长链多不饱和脂肪酸(n-3 LC-PUFA)模式。EC-UFA模式与ESCC风险增加相关,而n-3 LC-PUFA模式与风险降低相关。然而,在研究对象中观察到的MLC-SFA或SFA模式没有显著相关性。
这是第一项揭示中国人群膳食 FAP 与 ESCC 风险之间关系的研究。在我们的日常生活中,人们吃的食物是由各种脂肪酸组成的,而不仅仅是一种脂肪酸。因此,FAP分析能够反映实际的膳食质量,并总结各种膳食FAs的作用,具有重要的意义。与分析单一脂肪酸的传统方法相比,因子分析可以调查膳食成分之间的关系。
原文来源:
Hu C, Lin Z, Liu Z, et al. Dietary fatty acid patterns and risk of oesophageal squamous cell carcinoma. PeerJ. 2022;10:e13036. Published 2022 Mar 31. doi:10.7717/peerj.13036.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PE#
45
#癌风险#
37
#SCC#
39
#peer#
31
#食管#
31
#ESCC#
34