J Clin Oncol:强化局部放疗可改善局限性前列腺癌患者的疾病控制
2021-01-29 MedSci原创 MedSci原创
体外放射疗法(EBRT)治疗局限性前列腺癌的剂量反应关系已有概述。全前列腺剂量最高增加至80 Gy被认为是安全有效的。本研究旨在研究EBRT对肉眼可见肿瘤的病灶强化是否能提高局限性前列腺癌患者的生化无
体外放射疗法(EBRT)治疗局限性前列腺癌的剂量反应关系已有概述。全前列腺剂量最高增加至80 Gy被认为是安全有效的。本研究旨在研究EBRT对肉眼可见肿瘤的病灶强化是否能提高局限性前列腺癌患者的生化无病生存期(bDFS)。
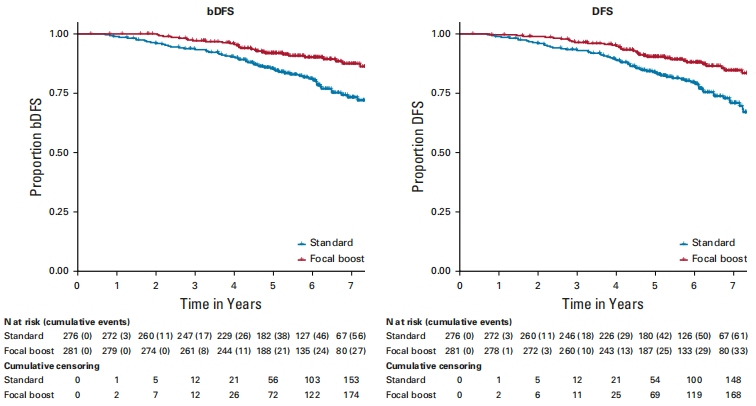
这是一项III期、多中心、随机对照的前列腺癌局部病灶消融性MicroBoost试验,在2009-2015年间招募了571名中高危前列腺癌患者,随机分组后,标准治疗组的患者整个前列腺接受了77 Gy(2.2 Gy/次)的放疗。病灶强化组同时接受了高达95 Gy(最高2.7 Gy/次)病灶强化放疗。主要终点是5年bDFS。次要终点是无病生存率(DFS)、无远处转移生存率、前列腺癌特异性生存率、总体生存率、毒性和与健康相关的生活质量。
中位随访了72个月。病灶强化组的生化DFS显著高于标准治疗组(危险比0.45,95% CI 0.28~0.71,p<0.001)。随访5年时,强化组和标准组的bDFS分别为92%和85%。前列腺癌特异性存活率和总存活率无显著差异(p分别为0.49和0.50)。标准组2级及以上晚期泌尿生殖系和胃肠道毒性的累积发生率分别为23%和12%,而强化组的分别为28%和13%。两组健康相关的生活质量的差异同样很小,没有统计学意义。
综上,对于前列腺内肿瘤病灶进行强化放疗,可在全前列腺标准体外放疗基础上进一步改善局部中高危前列腺癌患者的bDFS,且不会影响毒性和生活质量。该研究表明,病灶聚焦放疗增强策略可在不违背高危器官剂量限制性的同时改善肿瘤控制的方法有效且安全。
原始出处:
Kerkmeijer Linda G W,Groen Veerle H,Pos Floris J et al. Focal Boost to the Intraprostatic Tumor in External Beam Radiotherapy for Patients With Localized Prostate Cancer: Results From the FLAME Randomized Phase III Trial. J Clin Oncol, 2021, undefined: JCO2002873.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oncol#
34
#局限性#
31
#J Clin Oncol#点击查看更多该期刊内容
68
#局部#
35
#局限性前列腺癌#
52
谢谢梅斯分享这么多精彩信息
59
前列腺癌相关研究,学习了,谢谢梅斯
53
学到了
88
副作用大不大
79
全前列腺剂量最高增加至80 Gy被认为是安全有效的。
68