Cell Rep:肠道微生物大规模宏基因组研究突破,助力治疗心血管疾病!
2020-03-19 MedSci原创 MedSci原创
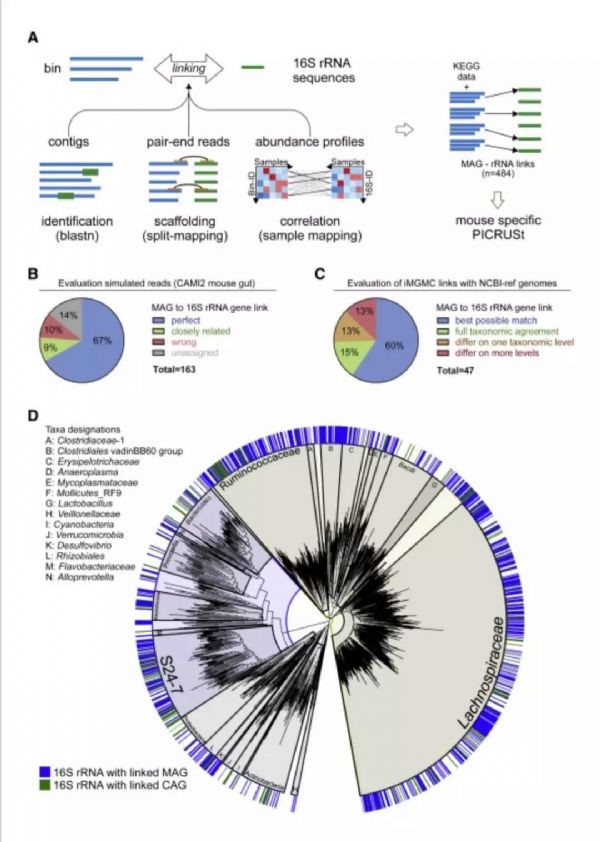
导语:肠道菌群是一个动态且高度多样化的微生物生态系统,会影响宿主生理的许多方面,虽然许多研究侧重于单个微生物分类群对机体健康的影响,但它们的整体代谢潜力尚未得到充分的探索。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cell#
29
#微生物#
22
#CEL#
27
#研究突破#
30
#大规模#
30
#宏基因组#
31
#血管疾病#
28