PRS:技术更新!三维成像设计条形颅骨切除术虚拟头盔
2021-03-16 MedSci原创 MedSci原创
传统头盔方案和虚拟头盔方案均改善了平均头颅指数,但虚拟头盔组的头颅指数变化更一致、更大。虚拟头盔设计方案产生了与年龄匹配的对照组相似的三维结果。与虚拟头盔组和对照组相比,传统头盔设计产生了更窄的双顶尺
微创条形颅骨切除术是治疗矢状缝颅缝畸形的安全有效的治疗方法。头盔疗法是矢状条形颅骨切除术后最常见的辅助手段,用于促进颅顶的被动重塑。颅骨的快速生长、颅骨的延展性、楔形截骨术的增加和头皮的顺应性使颅顶发生了快速的三维变化。在术后早期,头盔允许婴儿仰卧,头部的重量放在枕骨上,从而允许顶骨的被动侧向运动,从而促进颅顶的快速重塑。头盔还限制了不必要的过度垂直膨胀。矢状面融合的限制性和补偿性生长模式存在显著差异。矢状条形颅骨切除术后佩戴的头盔必须根据手术程序和患者的解剖结构定制,以确保不会因顶骨与头盔的任何部分意外接触而抑制被动扩张,以达到最佳效果。

这项研究比较了一种新的虚拟头盔设计和一种传统头盔设计所获得的三维头型结果,并将每组受试者与年龄匹配的对照组受试者进行了比较。
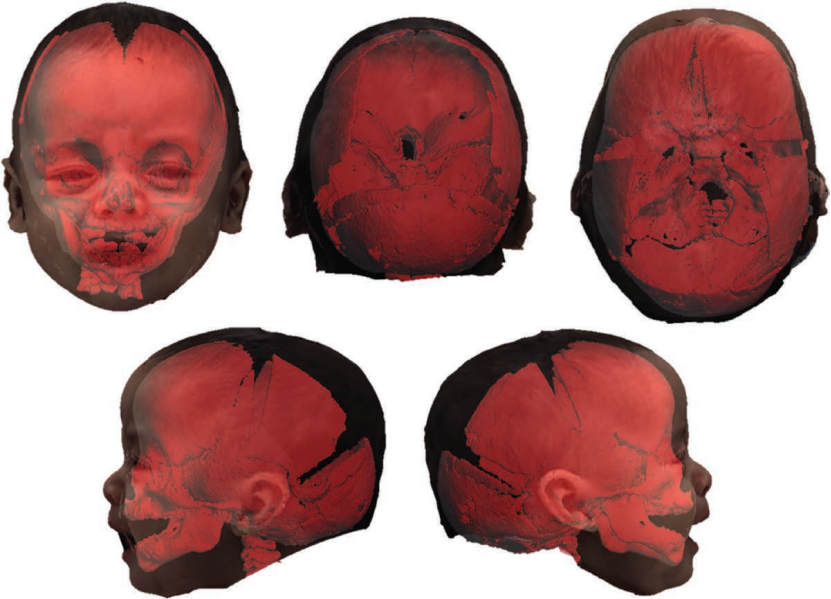
该研究共纳入24例患者。11名患者组成了传统的头盔组,基于激光扫描设计头盔。13名患者组成虚拟头盔组,基于低辐射方案计算机断层扫描和三维照片的三维体绘制叠加设计头盔。从三维照片上记录头颅指数和垂直高度。生成三维全头复合图像,以比较全球头型结果与年龄匹配的对照组的结果。
虚拟头盔组平均头颅指数(83.70±2.33)分与对照组(83.53±2.40)分比较,差异无统计学意义(P>0.05)。
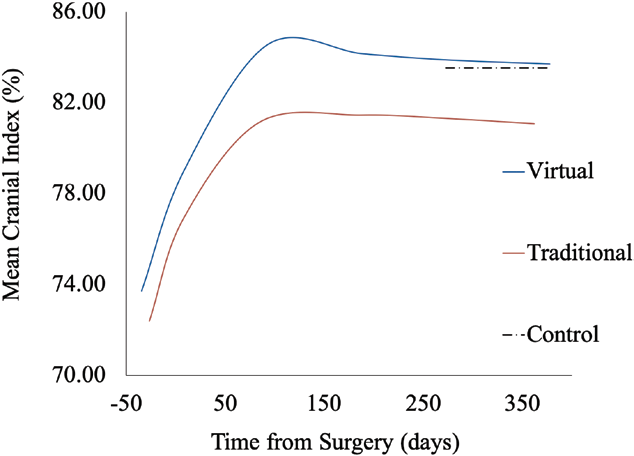
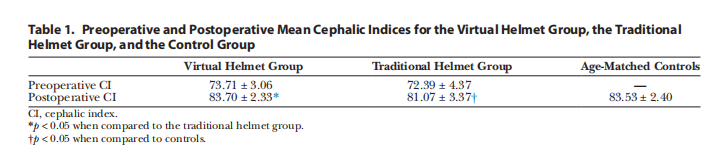
传统头盔组平均头指数(81.07±3.37)与对照组比较差异有统计学意义(P<0.05),平均垂直高度差异有统计学意义(P<0.05)。
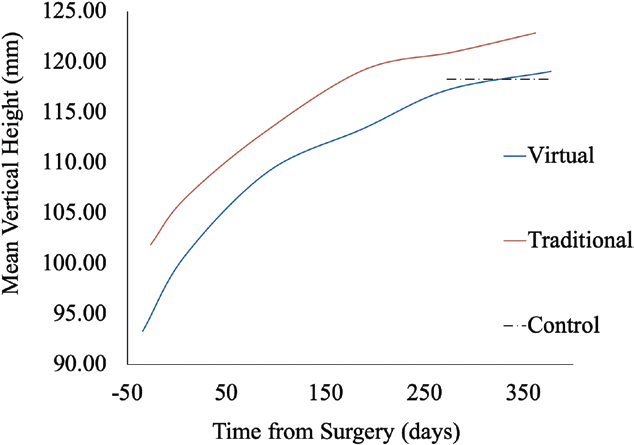
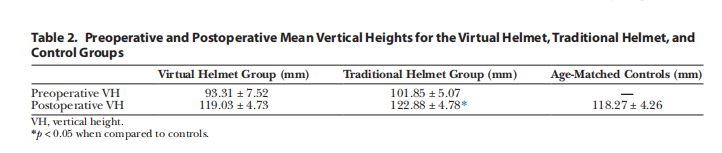
三维分析显示,与对照组相比,虚拟头盔组的双顶和垂直维度正常。与对照组相比,传统头盔组的双顶径较窄,垂直径较大。
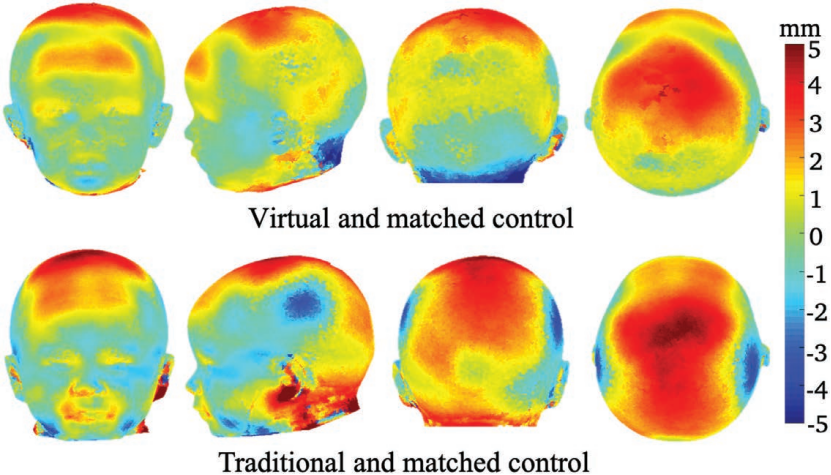
传统头盔方案和虚拟头盔方案均改善了平均头颅指数,但虚拟头盔组的头颅指数变化更一致、更大。虚拟头盔设计方案产生了与年龄匹配的对照组相似的三维结果。与虚拟头盔组和对照组相比,传统头盔设计产生了更窄的双顶尺寸和更大的颅顶垂直尺寸。这支持使用三维成像来评估矢状位颅缝融合症的治疗结果。
原始文献:
Ramamurthi Aishwarya,Hallac Rami R,Chou Pang-Yun et al. Three-Dimensional Treatment Outcomes of a Virtual Helmet Design Protocol for Sagittal Strip Craniectomy.[J] .Plast Reconstr Surg, 2021, 147: 436-443.
DOI: 10.1097/PRS.0000000000007642
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#三维成像#
35
#切除术#
24
#颅骨切除术#
27
#PRS#
23
厉害
67
学到了!
75