JAHA:新诊断的房颤和慢性肾病患者治疗与1年结局
2019-02-07 xing.T MedSci原创
由此可见,在GARFIELD-AF中,中度至重度CKD与卒中/全身性栓塞、大出血和死亡独立相关。亚洲患者的中度至重度CKD对死亡率的影响甚至超过世界其他地区。
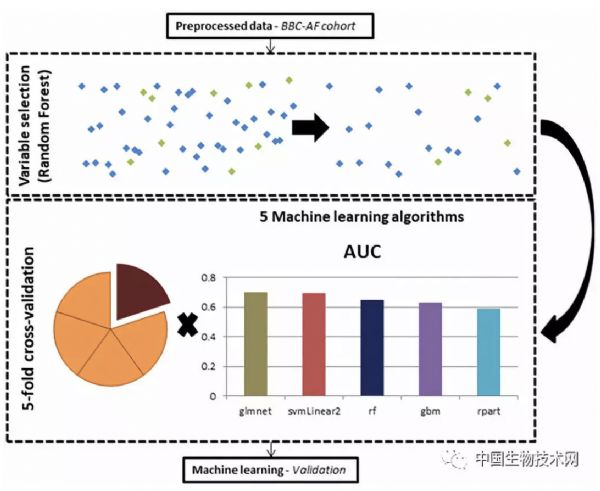
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员使用来自GARFIELD-AF(FIELD-房颤的全球抗凝血登记处)的数据,评估了慢性肾病(CKD)阶段对新诊断的心房颤动(AF)患者临床结局的影响。
GARFIELD-AF是来自35个国家患者的前瞻性登记中心,包括来自亚洲(中国、印度、日本、新加坡、韩国和泰国)的患者。根据国家肾脏基金会的肾病结局质量倡议指南将入选的连续就诊的患者(2013-2016)分类为无、轻度或中度至重度CKD。
34854名患者(包括来自亚洲的9491名患者)中有33024名患者获得了CKD状态和结局的数据;10.9%(n=3613)患有中度至重度CKD,16.9%(n=5595)患有轻度CKD,72.1%(n=23816)无CKD。口服抗凝剂的使用受卒中风险的影响(即CHA2DS2-VASc评分的事后评估),但不受CKD阶段的影响。维生素K拮抗剂的抗凝血控制质量与CKD分期无差异。调整基线特征和抗血栓形成后,轻度和中度至重度CKD均为全因死亡率的独立危险因素。中度至重度CKD独立地与卒中/全身性栓塞、大出血、新发急性冠状动脉综合征以及新的或恶化的心力衰竭的风险相关。亚洲患者中度至重度CKD对死亡率的影响显著高于世界其他地区(P=0.001)。
由此可见,在GARFIELD-AF中,中度至重度CKD与卒中/全身性栓塞、大出血和死亡独立相关。亚洲患者的中度至重度CKD对死亡率的影响甚至超过世界其他地区。
原始出处:
Shinya Goto.et al.Management and 1‐Year Outcomes of Patients With Newly Diagnosed Atrial Fibrillation and Chronic Kidney Disease: Results From the Prospective GARFIELD‐AF Registry.JAHA.2019.https://www.ahajournals.org/doi/full/10.1161/JAHA.118.010510
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#新诊断#
31
#慢性肾病患者#
33
#肾病患者#
40
#AHA#
38
学习
55