盘点:皮肤癌指南共识一览
2016-10-10 MedSci MedSci原创
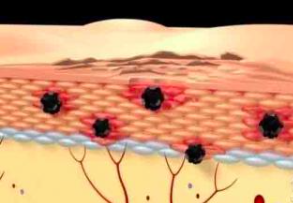
皮肤癌即皮肤恶性肿瘤,包括鳞状细胞癌、基底细胞癌、恶性黑色素瘤、恶性淋巴瘤、特发性出血性肉瘤、汗腺癌、隆突性皮肤纤维肉瘤、血管肉瘤等。皮肤癌有原发性癌和由其他部位转移至皮肤的继发性癌。原发性皮肤癌常见的有基底细胞癌、原位鳞癌(鲍温病)、鳞状细胞癌、湿疹样癌和恶性黑色素瘤。 皮肤癌病病因尚不明确,其发生可能与日光、化学致癌物质、慢性刺激与炎症、病毒致癌物质等因素有关,梅斯小编就为大家盘点一
皮肤癌即皮肤恶性肿瘤,包括鳞状细胞癌、基底细胞癌、恶性黑色素瘤、恶性淋巴瘤、特发性出血性肉瘤、汗腺癌、隆突性皮肤纤维肉瘤、血管肉瘤等。皮肤癌有原发性癌和由其他部位转移至皮肤的继发性癌。原发性皮肤癌常见的有基底细胞癌、原位鳞癌(鲍温病)、鳞状细胞癌、湿疹样癌和恶性黑色素瘤。
皮肤癌病病因尚不明确,其发生可能与日光、化学致癌物质、慢性刺激与炎症、病毒致癌物质等因素有关,梅斯小编就为大家盘点一下近期发布的最新皮肤癌指南与大家分享。
一 2017 NCCN临床实践指南:隆突性皮肤纤维肉瘤(2017.V1)
2016年10月3日,美国国家综合癌症网络(NCCN)更新了隆突性皮肤纤维肉瘤指南。(文章详见:2017 NCCN临床实践指南:隆突性皮肤纤维肉瘤(2017.V1))
二 2017 NCCN临床实践指南:皮肤鳞状细胞癌(2017.V1)
2017年10月3日,美国国家综合癌症网络(NCCN)发布了皮肤鳞状细胞癌2017年第一版。(文章详见:2017 NCCN临床实践指南:皮肤鳞状细胞癌(2017.V1))
三 2017 NCCN临床实践指南:皮肤基底细胞癌(2017.V1)
2016年10月3日,美国国家综合癌症网络(NCCN)发布了皮肤基底细胞癌临床指南2017年第1版。(文章详见:2017 NCCN临床实践指南:皮肤基底细胞癌(2017.V1))
四 2017 NCCN临床实践指南:默克尔细胞癌(2017.V1)
2016年10月3日,美国国家综合癌症网络(NCCN)更新了默克尔细胞癌指南。(文章详见:2017 NCCN临床实践指南:默克尔细胞癌(2017.V1))
五 2016 NCCN临床实践指南:皮肤基底细胞癌(2016.V2)
2016年5月,美国国家综合癌症网络(NCCN)发布了皮肤基底细胞癌临床指南2016年第2版,指南更新摘要如下: 皮肤基底细胞癌临床表现、检查和风险状态 皮肤基底细胞癌初始治疗和辅助治疗 皮肤基底细胞癌的随访和复发 皮肤基底细胞癌的治疗原则 皮肤基底细胞癌放射治疗(文章详见:2016 NCCN临床实践指南:皮肤基底细胞癌(2016.V2))
六 2016 USPSTF建议声明:皮肤癌筛查
2016年7月26日,美国预防医学工作组(USPSTF)更新发布了皮肤癌筛查建议,该建议的前一版于2009年发布,USPSTF指出现有证据不足以评估平衡目视皮肤检查对于成人临床皮肤筛查的风险和获益。(文章详见:2016 USPSTF建议声明:皮肤癌筛查)
七 2015 ESMO临床实践指南:皮肤黑色素瘤的诊断、治疗与随访
2015年9月,欧洲肿瘤内科学会(ESMO)发布了皮肤黑色素瘤的诊断、治疗与随访指南2015年版。(文章详见:2015 ESMO临床实践指南:皮肤黑色素瘤的诊断、治疗与随访)
皮肤恶性肿瘤如发现和治疗较早较恰当,一般来说,疗效和预后较好,但如已有区域性淋巴结转移者,则预后较差。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













很好很有帮助谢谢。
60
好文章,受益
84
一般来说,疗效和预后较好,但如已有区域性淋巴结转移者,则预后较差。
88
谢谢分享,
85
学习啦,
74
学习一下!
23
分享一下!
21
分享一下!
27
持续关注中
22