JAMA Neurology:机械取栓患者超时间窗也可选择CT平扫
2021-12-14 自由影像之光 MedSci原创
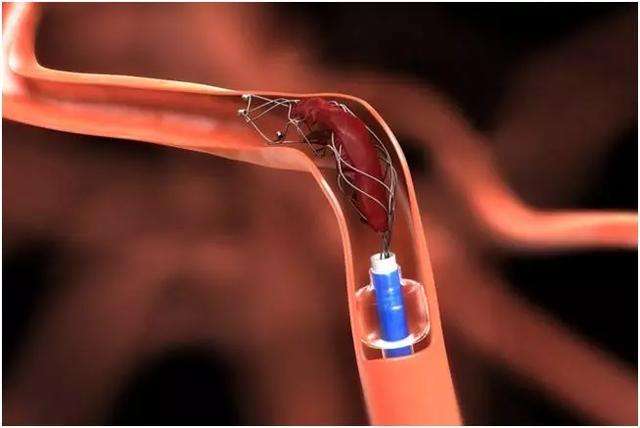
在机械取栓术中,先进的影像学检查并不能广泛应用。对于在超时间窗内出现近端前循环闭塞卒中的患者,选择非增强计算机断层扫描行血栓切除术的患者与选择计算机断层扫描灌注或磁共振成像的患者在90天时的良好预后率
在机械取栓术中,先进的影像学检查并不能广泛应用。对于在超时间窗内出现近端前循环闭塞卒中的患者,选择非增强计算机断层扫描行血栓切除术的患者与选择计算机断层扫描灌注或磁共振成像的患者在90天时的良好预后率是否具有可比性?
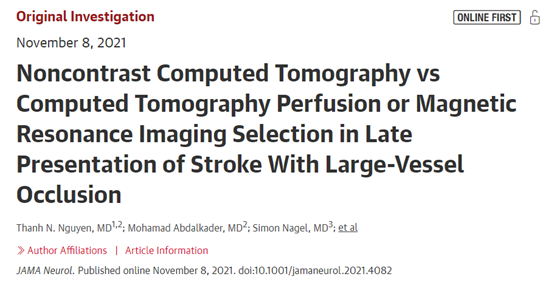
Thanh N. Nguyen等比较了超时间窗内非增强CT(CT)与CT灌注(CTP)或MRI(MRI)选择机械取栓患者的临床疗效,研究结果发表在JAMA Neurology杂志。
这项多国队列研究包评估了改良Rankin量表(mRS)评分在90天(顺序移位)的分布,90天功能独立比例(mRS评分为0-2)、症状性颅内出血和90天死亡率。
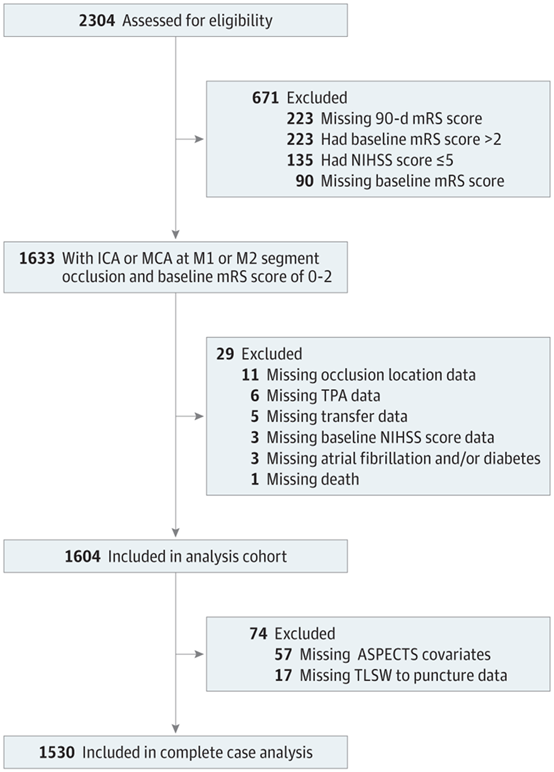
2304例患者中纳入1604例,中位年龄为70岁(59-80岁),848 (52.9%)为女性。共选择534例患者行CT机械取栓,752例行CTP,318例行MRI。调整混杂因素后,CT与CTP(调整比值比[aOR],0.95[95%CI,0.77-1.17];P=0.64)或CT与MRI(aOR,0.95[95%CI,0.8)选择的患者90天mRS位移无差异-1.13]; P=.55)。90天功能独立比例(mRS评分0-2 vs 3-6)在CT与CTP选择的患者之间相似(aOR,0.90[95%CI,0.7-1.16];P=.42),但MRI选择的患者低于CT(aOR,0.79[95%CI,0.64-0.98]; P=0.03)。

90天mRS分布变化情况
成功再灌注在CT和CTP组比MRI组更常见(474[88.9%]和670[89.5%]vs 250[78.9%]; P<0.001)。症状性颅内出血(CT,42[8.1%];CTP,43[5.8%];MRI,15[4.7%];P=0.11)或90天死亡率(CT,125[23.4%];CTP,159[21.1%];MRI,62[19.5%];P=0.38)无差异。
对于有颈内动脉和大脑中动脉(M1/M2段)大血管闭塞的患者,在症状出现后6 ~ 24小时内行机械取栓,非增强CT与先进的CTP或MRI相比,在临床和安全性方面没有显著差异。这些发现有可能扩大使用更简单、更便宜、更容易实现的非增强CT成像作为CTP或MRI的替代方案用于超时间窗治疗患者。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Neurol#
34
#超时间窗#
29
#取栓#
52
#CT平扫#
50
#机械取栓#
54