病例讨论:体检发现左肾下极占位1周
2015-12-11 丁玉芹 周建军 复旦大学附属中山医院放射科
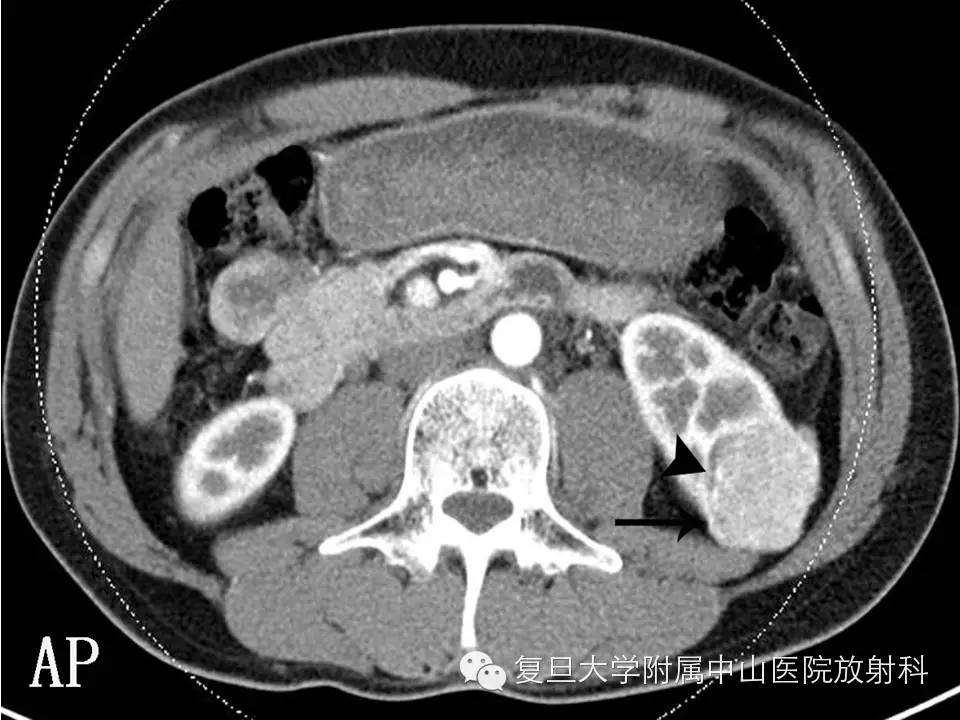
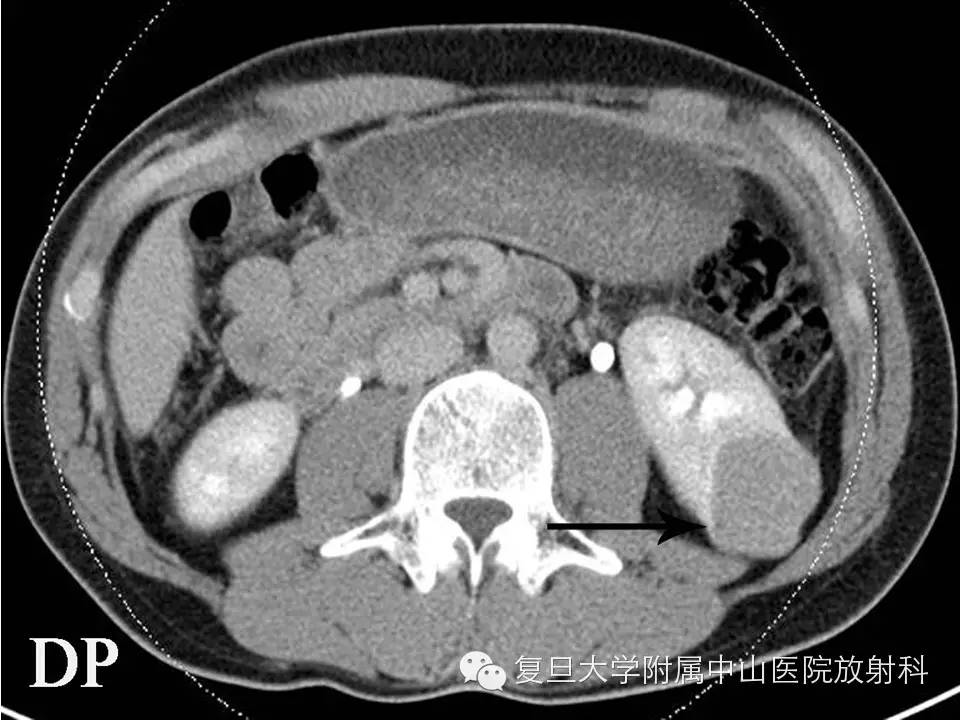
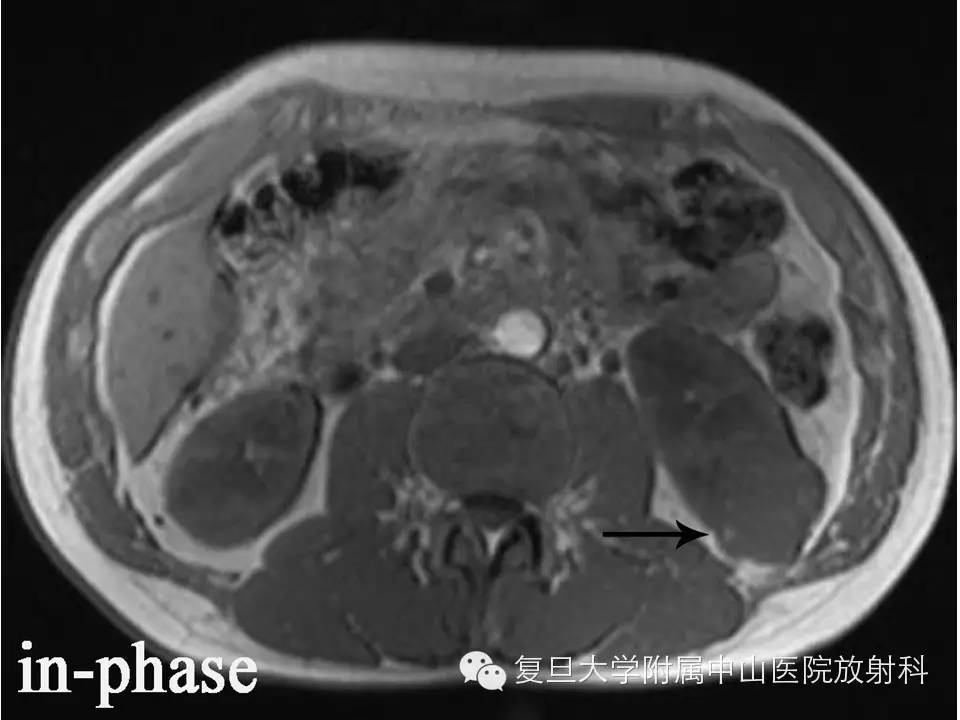
病史 男 ,39 ,因“体检发现左肾下极占位1周”入院,无发热、血尿、腰酸腰痛等症状。实验室检查:肾功能和肿瘤指标均正常。 肾脏CT和MRI平扫检查如下: 答案往下 {nextpage} CT和MRI表现 左肾下极可见一不规则软组织肿块影,平扫呈稍高密度,其右侧缘可见斑点状更低密度影(箭头,少量脂肪成分),增强后皮髓质交界期中等程度均匀强化,其右侧缘可见明显强化血管影(




本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#病例讨论#
37
很容易误诊,学习了,有类似病例可要注意了
98
多谢了
135
很值得学习,充电
126
典型案例,学习了。
98
…………
163
…………
33
#体检#
32
不错的病例,学习了。
谢谢分享!
105
医学加油!
27