Injury:真皮再生模板可有效治疗创伤性软组织缺损
2014-07-16 佚名 丁香园
严重创伤可造成广泛的软组织损伤,外科医生常常需要寻求新的的修复材料替代皮肤来闭合伤口。而这些修复材料需要保持真皮和表皮的基本功能和美观,它主要由动物Ⅰ型胶原纤维层和粘附在上面的硅凝胶膜层。前者是作为真皮再生模板(dermal regeneration template,DRT),后者是临时的人工表皮屏障。因为真皮再生模型可通过模板的血管重建生成血管层,所以它还可用于皮瓣覆盖修复组织缺损中的血管重建
严重创伤可造成广泛的软组织损伤,外科医生常常需要寻求新的的修复材料替代皮肤来闭合伤口。而这些修复材料需要保持真皮和表皮的基本功能和美观,它主要由动物Ⅰ型胶原纤维层和粘附在上面的硅凝胶膜层。前者是作为真皮再生模板(dermal regeneration template,DRT),后者是临时的人工表皮屏障。因为真皮再生模型可通过模板的血管重建生成血管层,所以它还可用于皮瓣覆盖修复组织缺损中的血管重建。
Jean-Maxime Alet教授等的研究结果显示,真皮再生模板的重建可有效治疗严重的软组织缺损,文章最近发表在Injury上。
该前瞻性研究纳入了2006年12月到2008年9月间在该院治疗的15名严重的开放性骨折患者(平均年龄44.3岁),均合并有软组织的损伤,包括损伤了腱旁组织的肌腱、骨膜被破坏的骨或者关节囊受损的关节等。所有患者均使用双层的Renskin真皮再生模板覆盖软组织缺损区,它包括由2mm厚的Ⅰ型胶原纤维层组成的多孔可渗透模型和用聚酯面料加固的200um厚的硅脂片。
首先对骨折部位部位进行复位,预防性静脉注射抗生素后,冲洗伤口和清除不能存活的组织,即完成伤口植入床的准备。然后,根据伤口的大小切出合适的真皮植入,植入的真皮不能出现皱褶和水泡。术后定期换药,密切观察伤口变化。当皮肤表面呈橙色或桃色,即表明新皮形成,立即把硅脂层去除后行刃厚皮复合移植(split-thickness skin graft,STSG)。
研究结果显示,15名患者均完成了18个月的随访,其中有99.3%完成了刃厚皮复合移植(STSG)治疗(图1)。植入真皮移植模板后到刃厚皮复合移植前这段时间发生的并发症有模板松动、血清肿、局部感染或局部水肿。而需要进行修复的患者比例由移植时的80%下降到随访结束时的20%,Vancouver瘢痕量表评分则一直下降至2.5分(图2)。手术医生和患者对术后功能和外貌客观评分均高于“满意”(图3)。
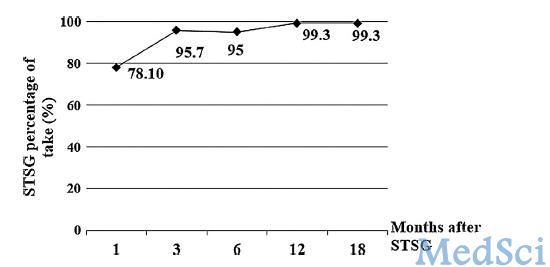
图:1:STSG治疗的比例
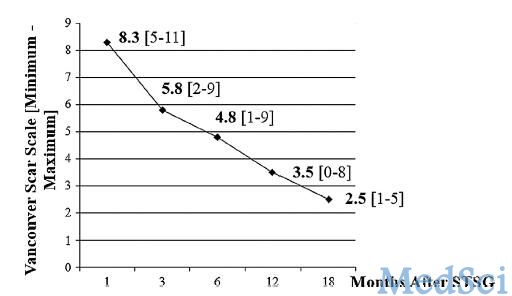
图2:Vanconver瘢痕量表
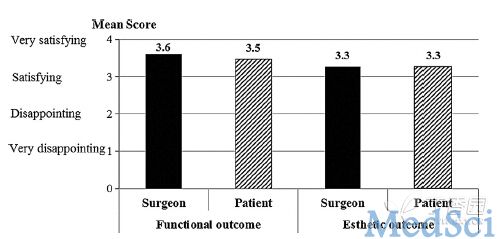
图3:患者和医生对功能恢复和美观情况的满意程度
总而言之,作者认为真皮再生模板治疗创伤性软组织损伤可获得良好的功能和美观恢复。
病例1:44岁男性,因摩托车事故发生右踝开放性骨折和脱位,合并有软组织损伤。行清创术,负压疗法治疗,暴露没有腱旁组织的肌腱(图5A)。然后,真皮再生模板植入(图5B),29天后行皮肤移植。2个月后,伤口愈合,无并发症发生(图5C)。18个月后评估受伤部位的功能和美观(图5D)。

案例2:63岁男性,车祸造成右踝软组织撕脱性损伤。行清创术后,负压疗法治疗,暴露肌腱和踝部的骨(图6A)。。然后,真皮再生模板植入(图6B),12天后行皮肤移植(图6C)。1个月后伤口愈合,18个月后踝关节功能恢复(图6D)。

原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Injury#
30
#创伤性#
33
#创伤#
34
#软组织#
37
#有效治疗#
31