病例1
-
女,62岁,因“突发意识不清2小时伴呕吐”急诊入院
-
既往史:1996年因右颞叶动静脉畸形行介入收入治疗,具体不详
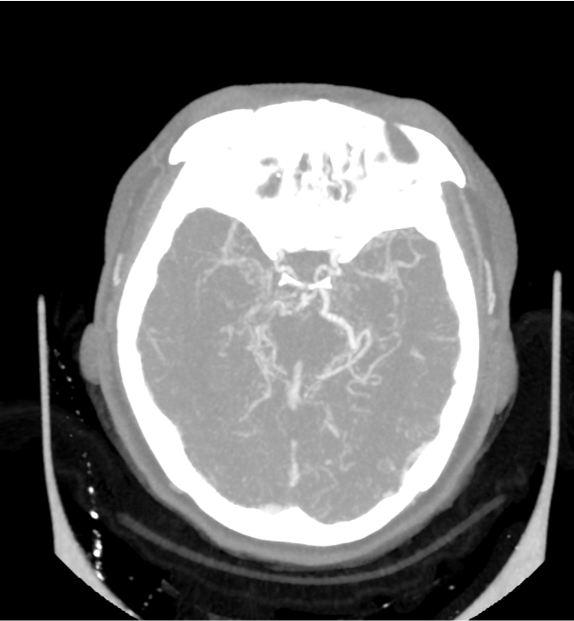
CT

病例2
-
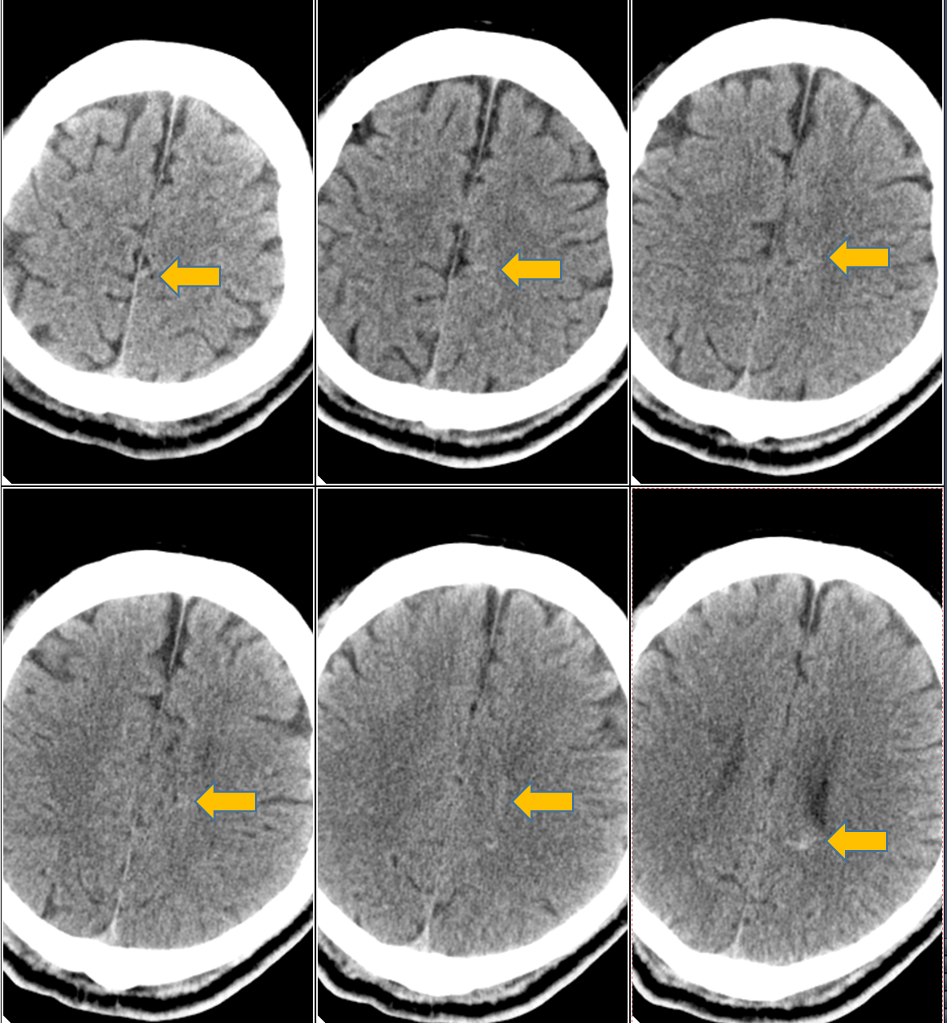
男,49岁,因“突发头痛7小时”急诊入院
-
患者自诉7小时前无明显诱因下出现额顶部头痛,呈持续性胀痛,至当地医院查头颅CT提示脑室出血,患者为求进一步诊治,转至我院急诊
CT+MRI


CTA


CT

CT+MRI





















版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#动静脉畸形#
37
#静脉#
37
#畸形#
33
很棒的课件
42
这个值得学习 收藏了 下次继续用
38