Lancet:通过遗传变异型预估冠心病风险
2015-03-05 姜英浩译 MedSci原创
目前的学界已经认识到,遗传变异与冠心病的发病风险密切相关。在本研究中,来自美国布莱根妇女医院与哈佛医学院的Mega医生领导的研究组进行了一项分析工作,验证遗传变异型中是否有组分能够协助判断冠心病的发病与复发的风险,并找出接受抑制素疗法临床疗效更好的人群。 该研究选取了1项基于社区的队列研究(the Malmo Diet and Cancer Study),4项随机对照试验包括了初级预防(JU
目前的学界已经认识到,遗传变异与冠心病的发病风险密切相关。在本研究中,来自美国布莱根妇女医院与哈佛医学院的Mega医生领导的研究组进行了一项分析工作,验证遗传变异型中是否有组分能够协助判断冠心病的发病与复发的风险,并找出接受抑制素疗法临床疗效更好的人群。
该研究选取了1项基于社区的队列研究(the Malmo Diet and Cancer Study),4项随机对照试验包括了初级预防(JUPITER、ASCOT),次级预防(CARE、PROVE IT-TIMI 22),均采用了抑制素疗法。研究共包含了48 421名受试者以及3477次发病事件。研究调整了传统的临床风险因素,并评估基于27个遗传变异型制订的遗传风险评分与冠心病发病和复发之间的联系。随后,本研究按基因风险进行分层,调查了接受抑制素疗法后的冠心病事件的相对和绝对风险降低值。通过meta分析将以上不同数据进行汇总。
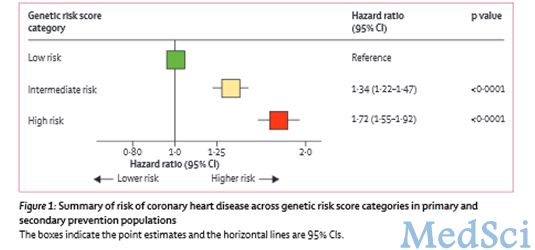
本研究将所有受试者按遗传变异型不同将其遗传风险分为5级,可以明显的将其冠心病发病或复发风险分出梯度。与低遗传风险组相比,中遗传风险组的冠心病多变量调整风险比(multivariable-adjusted hazard ratio)为1.34(95% CI 1.22–1.47, p<0.0001),而高遗传风险组则为1.72(1.55–1.92, p<0.0001)。而在所研究的4项试验中,抑制素疗法为各遗传风险组分别能够带来显著的相对风险降低,分别为低组(13 %),中组(29 %),高组(48 %)(p=0.0277)。同时,研究还发现在高遗传风险组的受试者中,绝对风险降低值也升高(p=0.0101),这导致了在初级预防试验中需要进行处理和预防冠心病的人数急剧降低了3倍。精确到具体数字来说,在初级预防试验JUPITER组中,10年内需要进行处理和预防冠心病的人数分别为低遗传风险组66人,中遗传风险组42人,高遗传风险组25人;在ASCOT组中分别为57、47和20人。
因此,研究人员认为,通过遗传风险评分可以评估个体冠心病发病和复发的风险水平。而对遗传风险高的人群给予抑制素疗法能够有效降低其相对和绝对临床疗效。
原文出处:
Jessica Mega, Nathan Stitziel, MDb, J Smith, et al. Genetic risk, coronary heart disease events, and the clinical benefit of statin therapy: an analysis of primary and secondary prevention trials. Lancet, 2015.3.4.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#冠心病风险#
34
#Lancet#
37
能个体化吗
176
#变异#
37
#遗传变异#
24
所谓的精准治疗吧
125
好文章,攒
113
好文章,攒
88
好文章,攒
103