III期临床研究CheckMate -816证实:纳武利尤单抗联合化疗作为可切除非小细胞肺癌患者新辅助治疗,可显著改善无事件生存期
2022-04-12 梅斯医学 梅斯医学
值得关注!
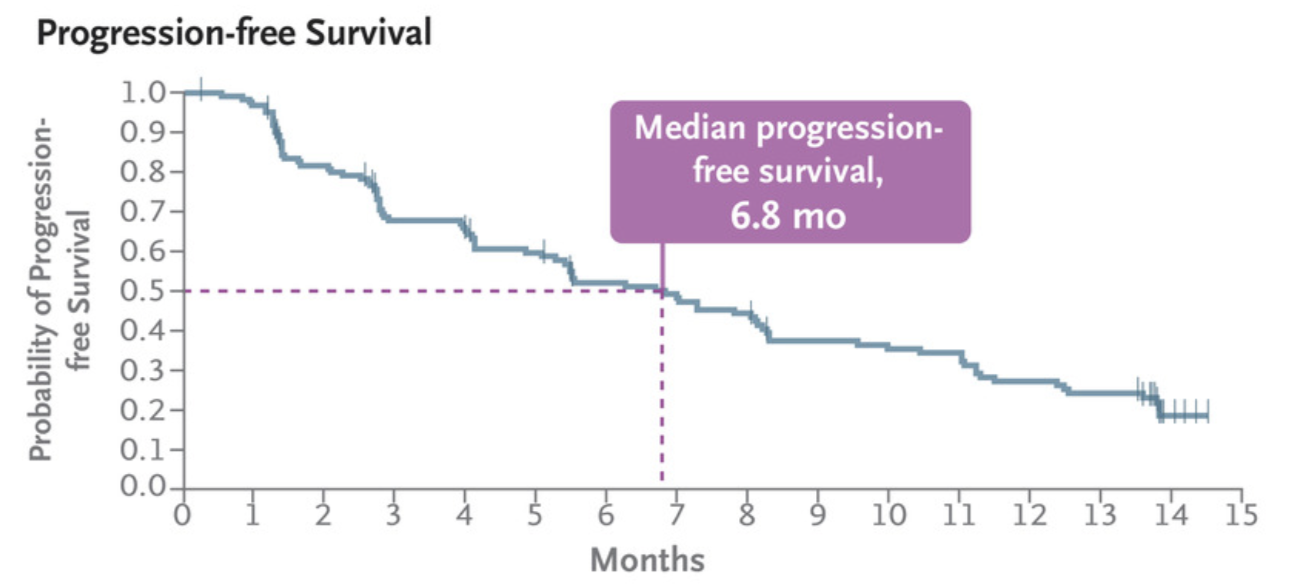
近日,百时美施贵宝(纽约证券交易所代码:BMY)公布了III期临床研究CheckMate -816主要研究终点无事件生存期(EFS)的数据。结果显示,与单用化疗相比,可切除非小细胞肺癌(NSCLC)患者在术前接受3个疗程的欧狄沃联合化疗,可显著改善患者EFS获益。患者随机分组,最短随访21.0个月时,术前接受纳武利尤单抗联合化疗的患者疾病复发、进展或死亡风险降低了37%(HR 0.63;97.38% 置信区间[CI]:0.43-0.91;p=0.0052)。纳武利尤单抗联合化疗组患者的中位EFS为31.6个月,而单用化疗组患者的中位EFS为20.8个月。
此外,虽然目前生存数据尚不成熟且分析未达到统计学边界,但在纳武利尤单抗联合化疗患者组中已观察到良好的总生存期(OS)早期获益情形(HR 0.57;99.67% 置信区间[CI]:0.30-1.07)。随访两年时,接受纳武利尤单抗联合化疗新辅助治疗的患者生存率为83%,在单用化疗患者中则为71%。后续会继续随访OS并做进一步分析。
CheckMate -816是首个证实以免疫为基础的联合治疗在新辅助阶段能够显著改善非小细胞肺癌患者EFS和另一主要研究终点病理完全缓解(pCR)率的III期临床研究。EFS数据于北京时间2022年4月11日23:15- 4月12日01:15在2022年美国癌症研究协会(AACR)年会新辅助和围手术期免疫治疗临床研究全体会议上首次公布(摘要编号#CT012),并同步在《新英格兰医学杂志》上发表。
CheckMate –816研究者、巴黎居里蒙苏里胸部研究所教授、所长Nicolas Girard博士表示:“尽管一些可切除非小细胞肺癌患者有治愈可能,但大部分患者仍然面临较高的术后复发风险,因此我们需要有效的系统性治疗方案来防止这一情况的发生。CheckMate -816 的研究结果首次证明,与单用化疗相比,以免疫治疗为基础的联合方案新辅助治疗能够为这些患者带来明确且显著的获益。在该研究中,我们首先观察到患者的病理完全缓解率获得了改善,如今又看到了无事件生存期的提高,同时总生存期也呈现出了积极的获益趋势。我们正向着治愈患者的最终目标不断努力,这些数据表明,纳武利尤单抗联合化疗有望为患者带来更好的长期生存结果。”
在该研究中,纳武利尤单抗联合化疗作为新辅助治疗的安全性与既往研究报道一致,在对EFS进行分析时未观察到新的安全性信号。与单用化疗相比,纳武利尤单抗联合化疗组3-4级治疗相关不良事件的发生率与单用化疗组相似(34% vs 37%)。此外, 3-4级手术相关不良事件在两组中的发生率也相似(纳武利尤单抗联合化疗组:11%,单用化疗组:15%)。纳武利尤单抗联合化疗组中83%的患者接受了手术,而单用化疗组为75%。
CheckMate -816研究者、麦吉尔大学外科学副教授、麦吉尔大学健康中心蒙特利尔总医院胸部和上消化道外科主治医师Jonathan Spicer表示:“手术仍然是治愈非小细胞肺癌患者的基石。纳武利尤单抗联合化疗作为新辅助治疗,使得手术时间更短、侵入性更小、手术范围更小,同时不增加并发症或不良事件,这对胸外科医生及其患者来说都是非常重要的。手术治疗结局的获益,加上对患者生存结果的改善,将有望彻底改变外科和肿瘤科医生在治疗可切除非小细胞肺癌患者时的合作方式。”
百时美施贵宝副总裁、胸部肿瘤开发负责人Abderrahim Oukessou博士表示:“免疫治疗开创了晚期癌症治疗的新时代,改变了肺癌和许多其他类型肿瘤患者的生存预期。近年来,随着对免疫系统和癌症生物学机理的深入了解,我们不断探索免疫治疗在新辅助、辅助和围手术期的使用。通过CheckMate -816的研究数据,包括令人鼓舞的总生存期早期结果,再次证实了在早期癌症中进行免疫治疗研究的重要性,我们期待继续看到这些科学研究能够为患者及其家人带来切实获益。”
基于CheckMate -816的EFS和pCR结果,美国FDA于2022年3月批准纳武利尤单抗联合含铂双药化疗(每三周一个疗程,共三个疗程),用于新辅助治疗肿瘤≥4cm或淋巴结阳性的可切除NSCLC成人患者。全球范围内的其他国家卫生监管机构也正在审评该新药上市申请。
在非转移性非小细胞肺癌领域,百时美施贵宝与合作伙伴正共同探索免疫治疗在新辅助、辅助和围手术期的使用,以及与放化疗的联用。在新辅助治疗阶段中使用肿瘤免疫治疗具有双重科学依据:首先,在采用免疫治疗时,肿瘤的存在可能会使免疫反应更强,从而有望使针对原发肿瘤的治疗更有效。其次,肿瘤免疫治疗将有机会清除隐蔽的微转移灶。迄今为止,欧狄沃作为新辅助或辅助治疗已在四种肿瘤类型中显示出了疗效改善,包括肺癌、膀胱癌、食管癌/胃食管连接部癌和黑色素瘤。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Checkmate#
44
#I期临床#
46
#肺癌患者#
62
#非小细胞#
42
#III期临床研究#
30
#III#
36
#II期临床研究#
29
#新辅助#
39
#生存期#
31
#联合化疗#
53