Nat Metab:杨巍维和姚烽团队合作发现肺癌免疫逃逸的代谢新机制
2022-03-22 网络 网络
中科院分子细胞科学卓越创新中心杨巍维课题组合作发现,MAPK等致癌信号通过调控丙酮酸脱氢酶PDHE1α的亚细胞转位促进肿瘤免疫逃逸。
中科院分子细胞科学卓越创新中心杨巍维课题组合作发现,MAPK等致癌信号通过调控丙酮酸脱氢酶PDHE1α的亚细胞转位促进肿瘤免疫逃逸。 北京时间2022年3月22日,国际学术期刊《自然—代谢》在线发表了这一研究成果。分子细胞卓越中心杨巍维研究员、赵允研究员和上海交通大学附属胸科医院姚烽副主任医师为该论文的共同通讯作者。杨巍维组张亚娟副研究员和博士研究生赵明为共同第一作者。
肺癌是全球癌症相关死亡的最常见原因,肺癌的治疗仍然是一个巨大的挑战。尽管针对免疫检查点的靶向治疗(抗PD-1治疗、抗PD-L1治疗等)在许多恶性肿瘤的治疗中展现出显著的成效,并且已经在晚期肺癌的治疗中发挥了重要作用,但并非所有PD-1阳性的肺癌患者都能从抗PD-1治疗中获益。解决肿瘤细胞对抗PD-1治疗的耐药性将具有重要的临床意义。
三羧酸循环(tricarboxylic acid cycle,TCA循环)是细胞中重要的代谢中枢,对于ATP的产生和许多生物合成途径中的前体的供应是必不可少的。尽管早期的研究认为癌细胞绕过TCA循环,主要利用有氧糖酵解;但新出现的证据表明,某些癌细胞,特别是那些原癌基因和抑癌基因表达不受控制的细胞,严重依赖TCA循环来生产能量和合成生物大分子。然而,TCA循环是否以及如何参与肿瘤免疫逃逸及抗PD-1治疗的耐药性仍不清楚。
在这项研究中,研究人员对肺癌患者的肿瘤组织进行了免疫荧光染色实验。意外的是,他们发现原本定位于线粒体基质、连接糖酵解和TCA循环的代谢酶,丙酮酸脱氢酶复合物E1组分α亚基(PDHE1α),存在丰富的胞质定位;胞质PDHE1α水平与病人的预后呈正相关。进一步的研究发现,胞质PDHE1α通过促进磷脂酶PPM1B对IKKβ S177/181(IKKβ激活的关键磷酸化位点)的去磷酸化削弱了NF-κB信号通路的激活,增强了炎症因子及细胞毒性T淋巴细胞(CTLs)诱导的肿瘤细胞死亡。
然而,MAPK等致癌信号(oncogenic signaling)的激活,导致胞质PDHE1α S327位点被ERK2磷酸化并转位到线粒体;胞质PDHE1α水平的下降恢复了NF-κB信号通路的活化;同时,线粒体PDHE1α的增多提升了α-酮戊二酸的含量,并促进炎症因子刺激下肿瘤细胞的ROS解毒。NF-κB的活化和ROS的清除共同促进了肿瘤细胞在炎症因子刺激下的存活,增强了肿瘤细胞对CTLs的耐受性,最终促进了肿瘤的免疫逃逸和抗PD-1治疗的耐药性。
此外,肺癌患者肿瘤组织中PDHE1α S327磷酸化水平与胞质PDHE1α水平、ERK2活性和NF-κB激活相关;胞质PDHE1α水平或PDHE1α S327磷酸化水平与肺癌患者的恶性程度和预后相关。
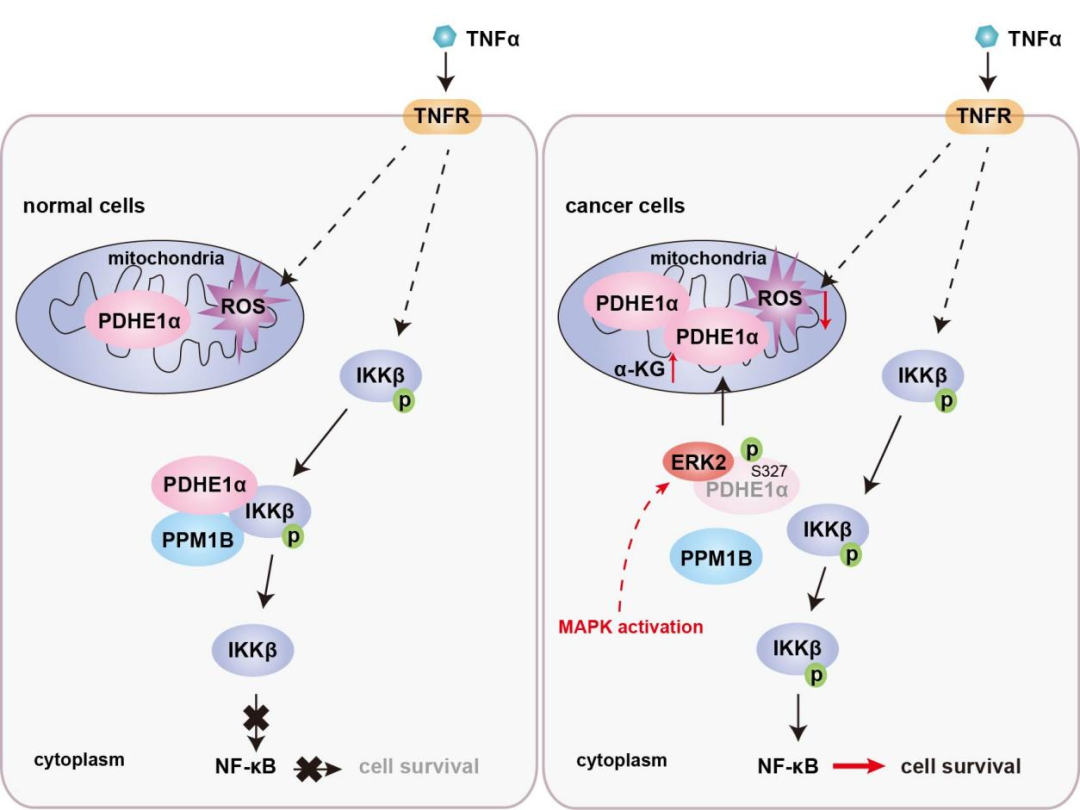
图:MAPK信号诱导的PDHE1α的磷酸化和转位促进肿瘤免疫逃逸
该工作发现了PDHE1α亚细胞转位在肿瘤免疫逃逸中的新功能;揭示了磷酸化调控PDHE1α亚细胞转位及PDHE1α亚细胞转位调控肿瘤免疫逃逸的新机制;提示了抑制PDHE1α的磷酸化可以阻断肿瘤的免疫逃逸并提高肿瘤免疫治疗的疗效。
该项研究工作得到了国家重点研发计划项目、国家自然科学基金、中国科学院青年基础研究项目等资助。
原始出处:
Zhang, Y., Zhao, M., Gao, H. et al. MAPK signalling-induced phosphorylation and subcellular translocation of PDHE1α promotes tumour immune evasion. Nat Metab (2022). https://doi.org/10.1038/s42255-022-00543-7https://www.nature.com/articles/s42255-022-00543-7
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
50
#Meta#
28
#MET#
47
太厉害了
61